Tick-borne Bourbon virus may have already infected many in St. Louis area

by Jacquelyn Kauffman, Washington University in St. Louis
On a cold spring morning, Washington University in St. Louis virologist Jacco Boon, PhD, and wildlife ecologist Solny Adalsteinsson, PhD, flap and drag a large white flag through a woodsy area on the western edge of St. Louis County.
Boon, an associate professor of medicine in infectious diseases at Washington University School of Medicine in St. Louis, and Adalsteinsson, a senior scientist at the university’s Tyson Research Center, are looking for lone star ticks that carry the potentially deadly Bourbon virus.
Earlier this year, the two — along with David Wang, PhD, the Robert C. Packman Professor of Molecular Microbiology at the School of Medicine — published a paper in the journal Ticks and Tick-borne Diseases showing that about one out of every 150 lone star ticks in the St. Louis area carries the virus.
In combing the woods for the minuscule yet potentially perilous arachnids, the researchers hope to learn more about where Bourbon virus-carrying ticks are located to better understand how the virus travels through wildlife and to people.
The technique — known as tick flagging — looks strange, but it works. After about 15 minutes of flapping and swiping in the university’s woodsy Tyson Research Center, an environmental field station for faculty, staff and students, Adalsteinsson stops and carefully plucks a single black dot from the cloth with a pair of forceps.
Lone star ticks
It’s a lone star tick, so tiny it’s barely visible between the delicate metal tips. They take it inside to Adalsteinsson’s research lab for further study.
“Tick-borne diseases are becoming more common. There are multiple reasons for this,” Boon said. Since he first started studying Bourbon virus, Boon has received more than $4 million in grant funding from the National Institutes of Health (NIH). He is the principal investigator on two NIH grants and a co-investigator on another two grants to study the virus.
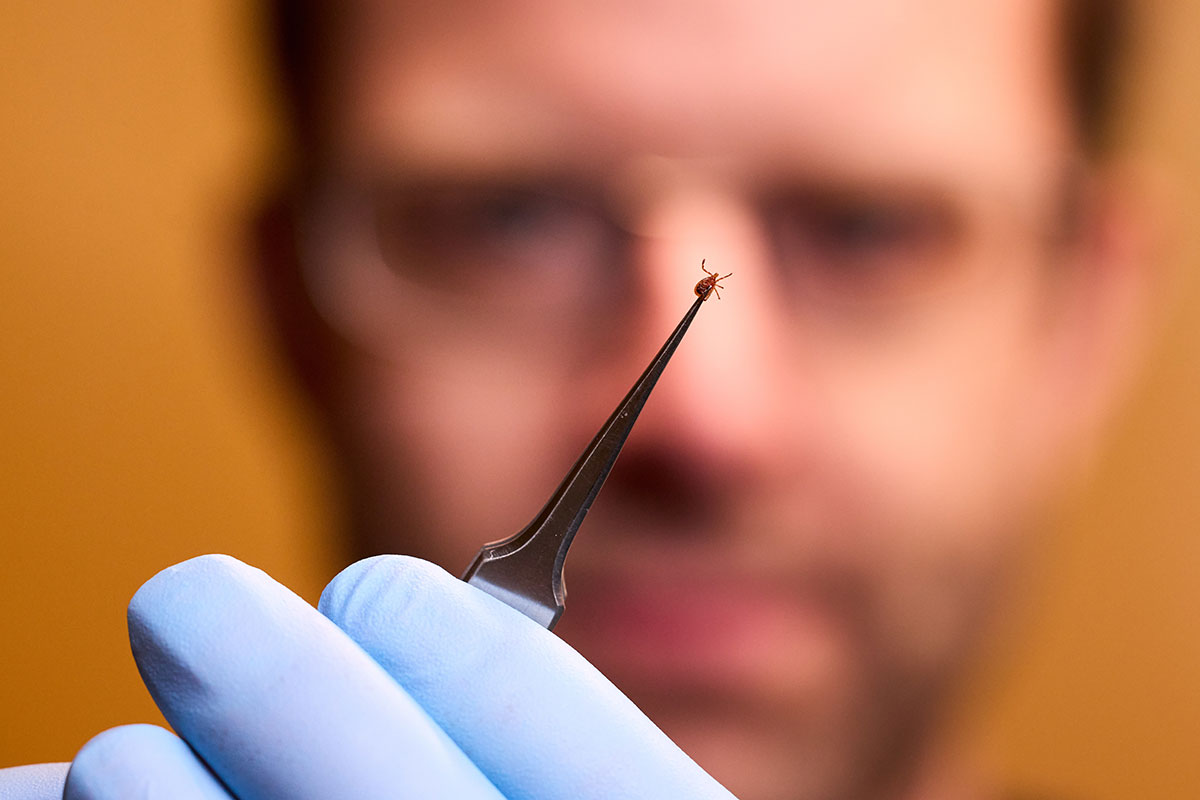 Jacco Boon holds a lone star tick collected at Washington University’s Tyson Research Center. Lone star ticks can carry the potentially deadly Bourbon virus. Boon and his colleagues are studying this virus and how it travels through wildlife and to people. (Matt Miller)
Jacco Boon holds a lone star tick collected at Washington University’s Tyson Research Center. Lone star ticks can carry the potentially deadly Bourbon virus. Boon and his colleagues are studying this virus and how it travels through wildlife and to people. (Matt Miller)“With climate change, winters are milder, and more ticks survive the winter,” he continued. “Urban areas are going green, which is a good thing, but all this new green space attracts white-tailed deer and coyotes, and with them come the ticks. My expertise is in virology, but since I’ve begun working on Bourbon virus, I’ve come to realize that the only way we are going to understand and address the problem of tick-borne viruses is if we also understand what is going on in the environment and among the wild animals that carry the ticks.”
The virus was named for the place it emerged: Bourbon County, Kansas. The first case was found there in 2014, in a man who died of the illness.
Since then, there have been only four more documented cases, including another death – statistics that make Bourbon virus look rare but lethal.
Many have antibodies
However, a study Boon published last year in the journal mSphere showed that a surprisingly high percentage of people in the St. Louis area have antibodies to Bourbon virus, suggesting that many people may have been infected and never known it.
To understand how the newly identified virus affects people in the St. Louis area, Boon collaborates with Adalsteinsson and Sharon L. Deem, DVM, PhD, a wildlife veterinarian and epidemiologist at the Saint Louis Zoo.
This triad of researchers represents a commitment to One Health, or the framework that human health is intertwined with the health of animals and the environment.
The first evidence of Bourbon virus’s presence in the St. Louis area came in 2017, when a woman was admitted to Barnes-Jewish Hospital with a fever, rash and body aches that turned out to be caused by Bourbon virus. There is no specific treatment for Bourbon virus infection — finding an effective therapy is something Boon is still working on — and she ultimately died of the illness.
Boon and his team cultured the virus from the St. Louis patient and used it to develop a mouse model of infection, which allowed them to study how the virus behaves in the body. The mouse model also helped lead to a potential drug therapy, although the drug in question has not progressed to clinical trials. The researchers also developed a way to test for antibodies to Bourbon virus in the blood.
“We have now tested blood samples from 1,500 people in the St. Louis area,” Boon said, referring to the mSphere study. “Out of those 1,500 random individuals, five have antibodies against Bourbon virus. That’s a very low number, but it is a very significant number still, because this means that Bourbon virus infection is much more common than we previously thought.”
The fact that it was so easy to find another five infections suggests that many people have probably been infected without becoming seriously ill, Boon said.
People get infected with Bourbon virus when they are bitten by a lone star tick that has acquired the virus from an infected animal. Deem’s portion of the project is focused on understanding how local wildlife may be affected by the virus and how they may play a role in the epidemiology of the virus.
Looking for wildlife hosts
“Our work is revealing information that is key to understanding the epidemiology of emerging pathogens that may threaten wildlife conservation and human health,” Deem said. “We can achieve this by getting a handle on how pathogens move through wildlife species in the area, and how animals may serve as hosts to ticks and viral pathogens.”
Deem leads a collaborative initiative based at the Tyson Research Center that includes the zoo, Washington University and the Endangered Wolf Center, a wolf-conservation nonprofit located on property owned by the Tyson Research Center. The initiative is dedicated to studying the movement of local carnivores such as foxes, coyotes and bobcats, and the diseases they carry.
During the colder months, Deem’s team traps animals and examines them, including taking blood samples to test for various infections. Then they mark and sometimes place a tracking device on the animals before letting them go unharmed. Bourbon virus antibodies have been found in most of the animal species trapped. The team also collects ticks straight from the animals trapped, and the presence of Bourbon virus is studied within these ticks as well.
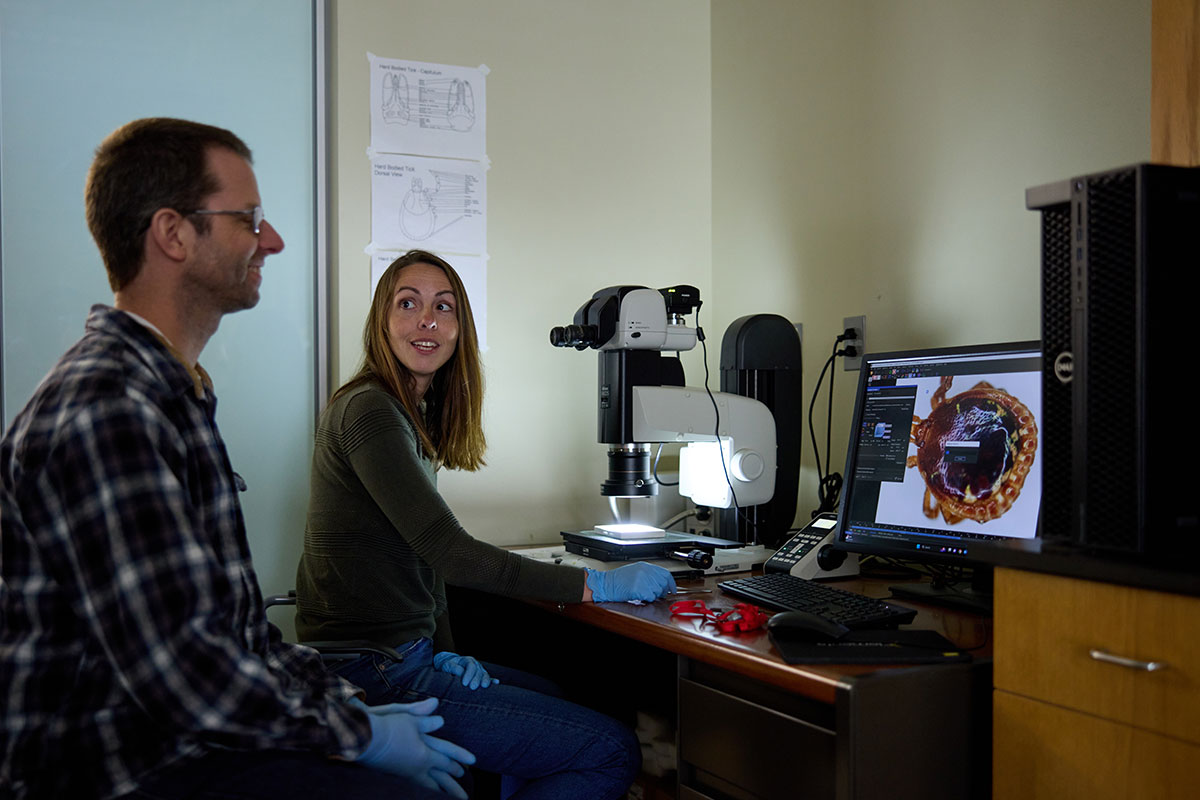
Meanwhile, Adalsteinsson collects ticks from the environment along with detailed data about the habitat characteristics and wildlife community nearby, and coordinates collections of blood and ticks from hunter-harvested deer.
She sends the ticks she’s collected to Boon’s lab to be tested for Bourbon virus. With Boon’s help, Adalsteinsson has been able to identify hot spots at Tyson, or geographical areas with a high proportion of Bourbon-positive ticks.
What drive transmission?
By identifying the environments that are most conducive to tick species or Bourbon virus proliferation, she hopes to understand more about what drives transmission.
“I am interested in connecting concepts from ecology and conservation to human health,” Adalsteinsson said. “There are many aspects of tick biology and tick-borne diseases that show explicitly how the way humans interact with and manage their environment can impact their own health.”
There is much work left to be done. Boon is working on learning more about the basic biology of the virus, such as how it gets inside cells, as a first step toward developing drugs and vaccines.
In the future, the interdisciplinary One Health team aims to understand more about how the virus spreads through wild animals, and where and how animals and people are getting infected. One goal is to identify the so-called reservoir species, the animal species that harbors the virus and keeps it in circulation.
Such information is crucial for designing effective intervention strategies. Another goal is to find out how long it takes for a tick to transfer the virus to a person, which will inform how frequently people need to check themselves for ticks.
“There is still so much we don’t know,” Adalsteinsson said. “We know the tick species that is transmitting the virus, but we don’t know which wildlife hosts might be involved in their maintenance. We don’t know the full extent of the range where they might occur. We have a lot of basic questions, and by bringing together our complementary expertise, we are making progress toward finding answers.”
SOURCE: Washington University in St. Louis




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page