“Words matter.” A new way of thinking about long-haul diseases.
“Infection-associated chronic illness” sounds like a mouthful.
But using that name has turned out to be a crucial first step in getting scientists, health officials, doctors, patients, and the public at large to think differently about ailments that can keep people sick for years—with few or no options for getting better.
For decades, people who remained ill after contracting Lyme disease, multiple sclerosis, ME/CFS and other poorly understood chronic conditions typically found themselves shunted aside by the medical establishment—often told they weren’t even sick. Federal support for researching better diagnostics and treatments for these disorders (or sometimes even acknowledging their existence) was minimal at best.
And then the COVID pandemic hit. Before long, it became clear that some people survived the disease but continued to suffer profoundly debilitating symptoms. Soon, the term “long COVID” entered the public vocabulary. Experts estimate the condition has forced 1.6 million full-time workers out of the US labor market, with significant ripple effects throughout the economy and society at large.
Shifting the paradigm
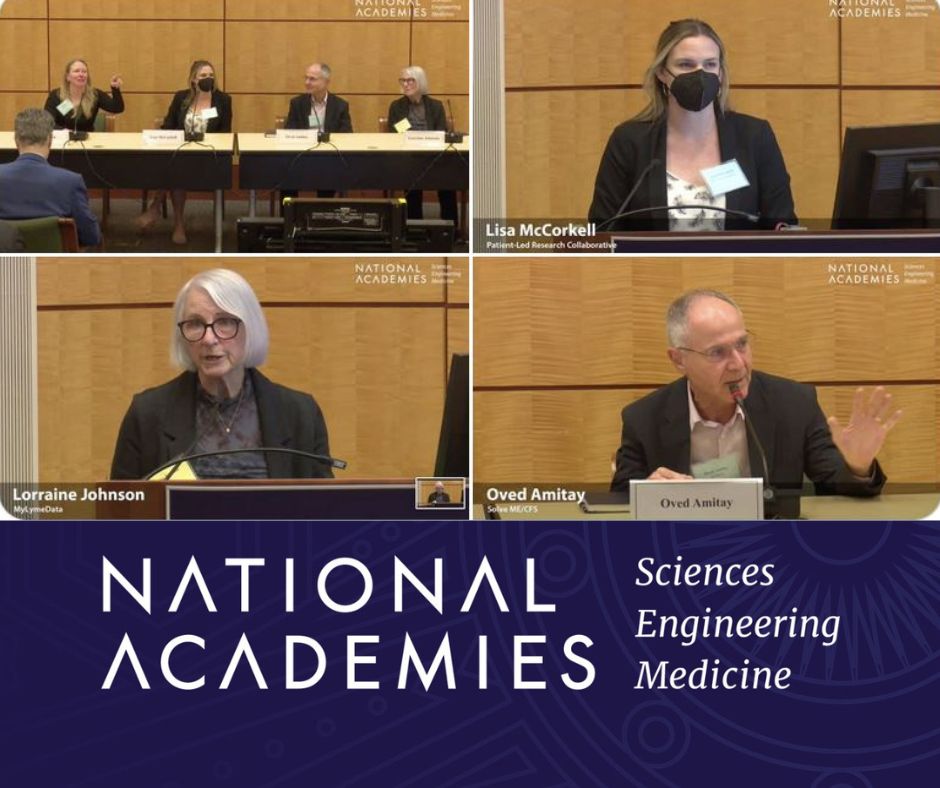
Fast-forward to June 29-30, 2023. The National Academies of Sciences, Engineering, and Medicine held a paradigm-shifting event in Washington DC titled “Toward a Common Research Agenda in Infection-Associated Chronic Illnesses: A Workshop to Examine Common, Overlapping Clinical and Biological Factors.”
It brought together high-level health officials, prominent researchers, and knowledgeable patient advocates from around the country. Their shared goal was to find a way to work collaboratively for the benefit of all these “long haul” patients.
The presentations were enlightening, inspiring and immensely gratifying. As chronic illness author Meghan O’Rourke highlighted in her opening remarks, “When I was very sick, I really did lie in my bed and wish that someday a group of scientists might come together to take interest in the plight of all of us who live with infection-associated illness.”
And here they all were, in one place, paying rapt attention to the results of patient-led research, presented by Hannah Davis and Lisa McCorkell (long COVID) and Lorraine Johnson (Lyme disease).
In addition, academic researchers delivered presentations on various factors relevant to all infection-associated diseases, including immune dysfunction, autonomic dysfunction, brain inflammation, and the role of the microbiome.
Discussions explored the strong connection between Epstein-Barr virus and multiple sclerosis, the persistence of pathogens in COVID-19 and Lyme disease, and the occurrence of postural orthostatic tachycardia syndrome (POTS) in both ME/CFS and long COVID. (We know that POTS is experienced by lots of folks with Lyme as well.)
Other speakers looked at possible treatments, including repurposing current drugs as well as developing new ones, along with better ways of helping patients cope with pain and fatigue.
Breaking down the silos
The various presentations demonstrated that there’s already a wealth of valuable information out there—but much of it is locked up in research silos. The term “silo” originally meant a tower for storing grain. Now it’s used metaphorically to describe organizations that operate independently and keep their discoveries to themselves.
There seemed to be consensus in the group for abolishing the silos and moving forward cooperatively. After a speaker floated the idea of creating a division of the National Institutes of Health devoted specifically to infection-associated chronic illness, an affirmative buzz moved through the audience.
Later, Rear Admiral Michael Iademarco, a high-ranking official at the Department of Health and Human Services, commented near the close of the event that “words matter.”
I wholeheartedly agree with that assessment. Uniting all these conditions under the term infection-associated chronic illness could be precisely what’s needed to make progress.
We are at a turning point. National health officials and research institutions are finally poised to give these debilitating conditions the attention they deserve. It’s what the patient community has long been fighting for.
I feel hopeful in a way I haven’t felt before.
This event was put together with major support from the Steven and Alexandra Cohen Foundation, which has long supported Lyme disease research. The community owes them a huge debt of gratitude.
Click here to watch video replay of the workshop.
TOUCHED BY LYME is written by Dorothy Kupcha Leland, President of LymeDisease.org. She is co-author of When Your Child Has Lyme Disease: A Parent’s Survival Guide. Contact her at dleland@lymedisease.org.























We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page