MEDICAL DETECTIVE #3: Let’s Talk About Lyme Rashes

This article was originally posted on Dr. Richard Horowitz’s Medical Detective Substack. You can find more helpful content by subscribing here.
The accuracy of Lyme testing has always been a problem, and testing recommendations that are FDA-approved are not always helpful. Actually, that is the understatement of the decade!
As you learned in the previous articles, there are over 100 different strains of Lyme disease in the US, and 300 strains worldwide.
Not all of them are pathogenic, but too many of them are—which is why we are in the middle of a worldwide epidemic of Lyme disease. According to BMJ Global Health, 14.5% of the world’s population has now been exposed to the disease (approximately 1/7 people living on the planet), but testing hasn’t caught up.
You’re never lucky if you get bitten by an infected tick, but your luck can improve if you notice a particular kind of rash, which makes testing easier.
Take a Look at Lyme Rashes
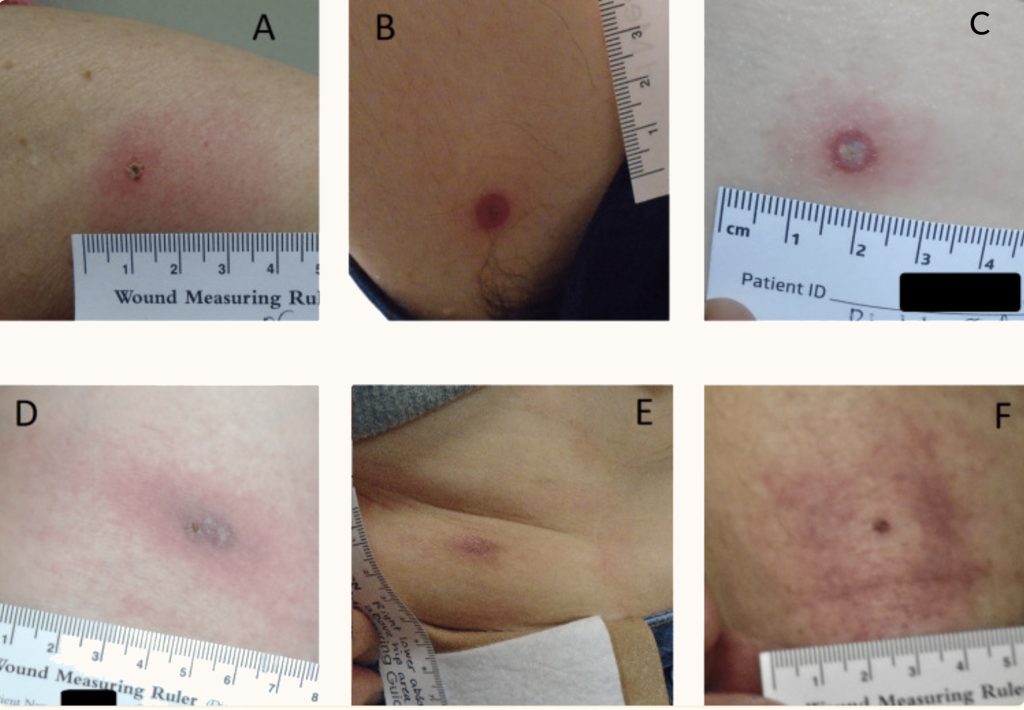
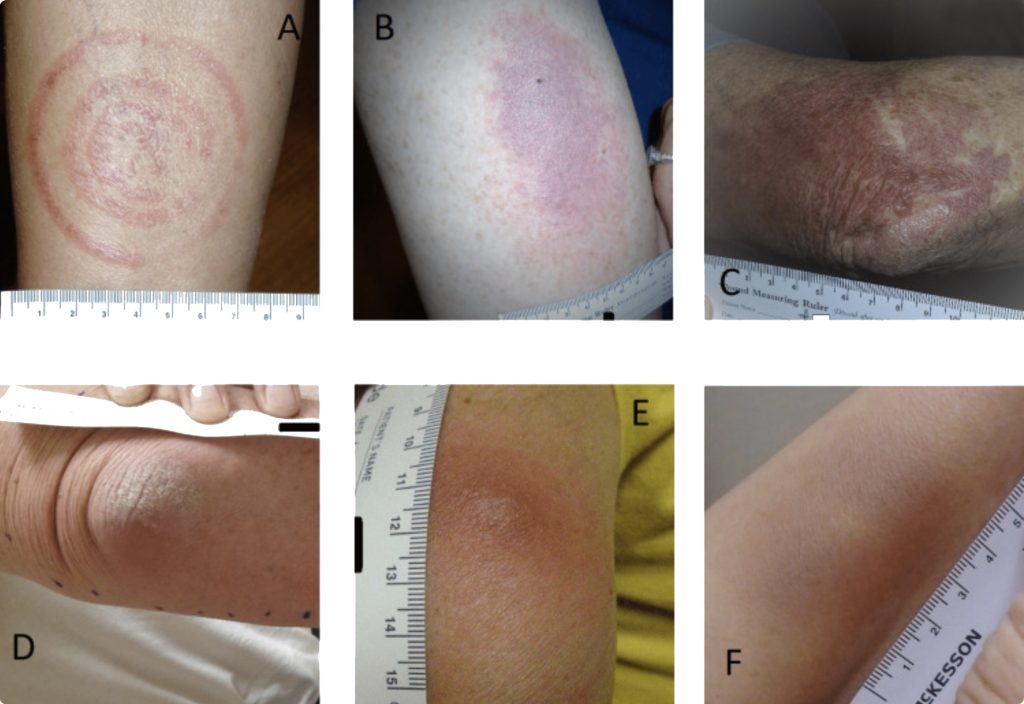
The most well-known rash is called an erythema migrans (EM). It looks like a bull’s-eye 50% of the time, but has multiple other shapes and sizes.
[Images courtesy of: Schotthoefer AM, Green CB, Dempsey G, Horn EJ. The Spectrum of Erythema Migrans in Early Lyme Disease: Can We Improve Its Recognition? Cureus. 2022 Oct 25;14(10):e30673. doi: 10.7759/cureus.30673. PMID: 36439577; PMCID: PMC9687974.]
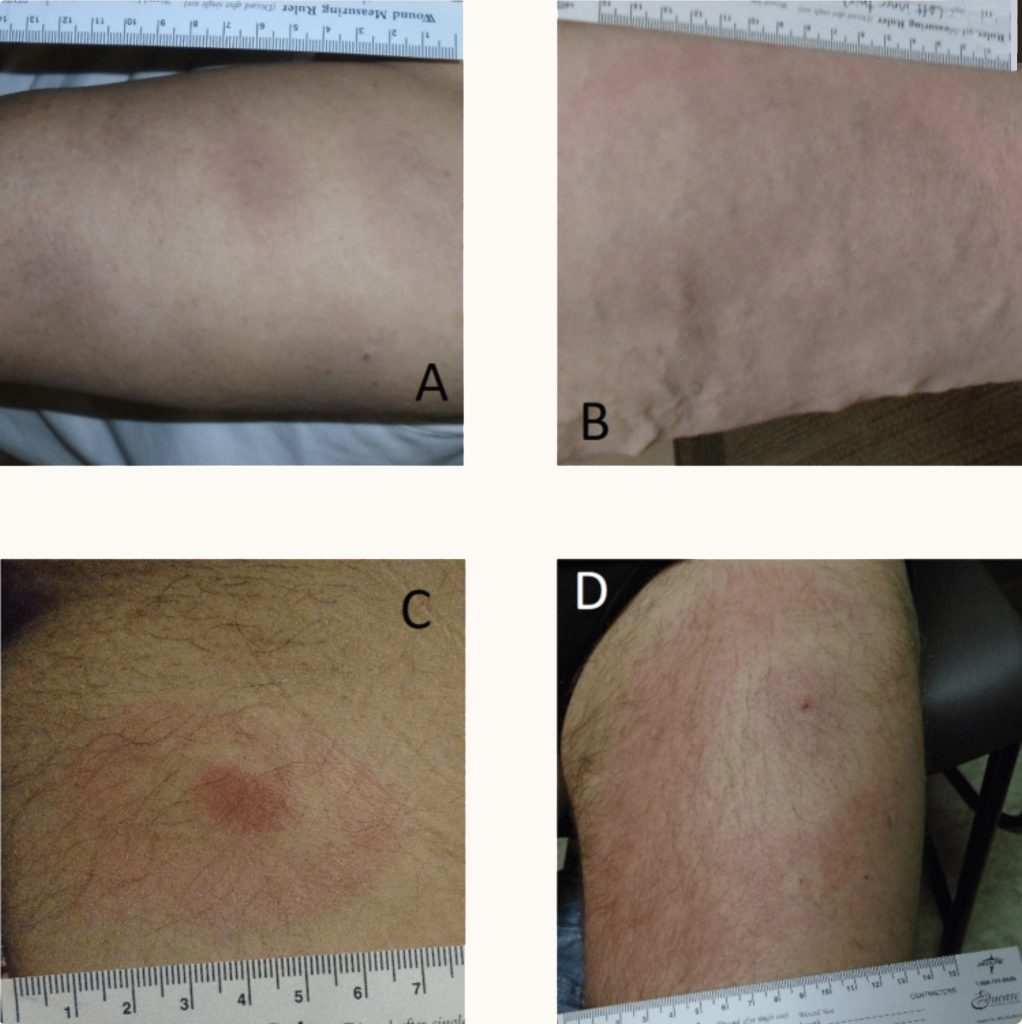
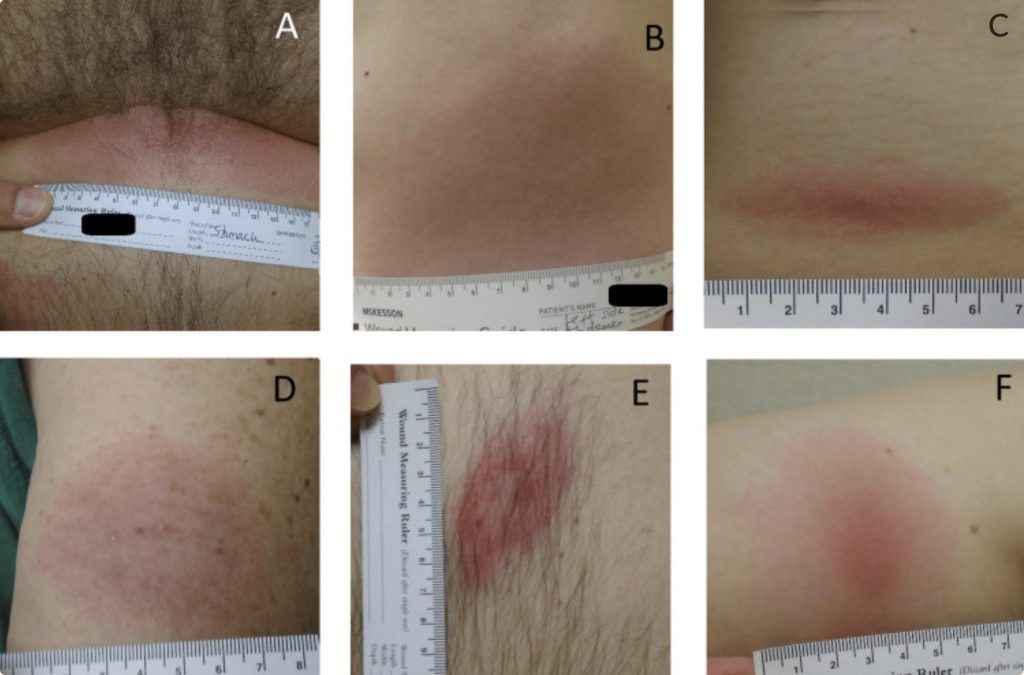
If you live in the US, Lyme rashes would include not only bull’s-eye rashes, but solid, spreading rashes that may be confused with a cellulitis (a bacterial skin infection from staph or strep), raised rashes, rashes that are bluish with vesicles in the centers (which can be confused with shingles and spider bites).
If you live in the Midwest, and get a strain of Lyme called Borrelia mayonii, the rash may be diffuse involving the face, trunk, and extremities. This could be confused with an allergic reaction.
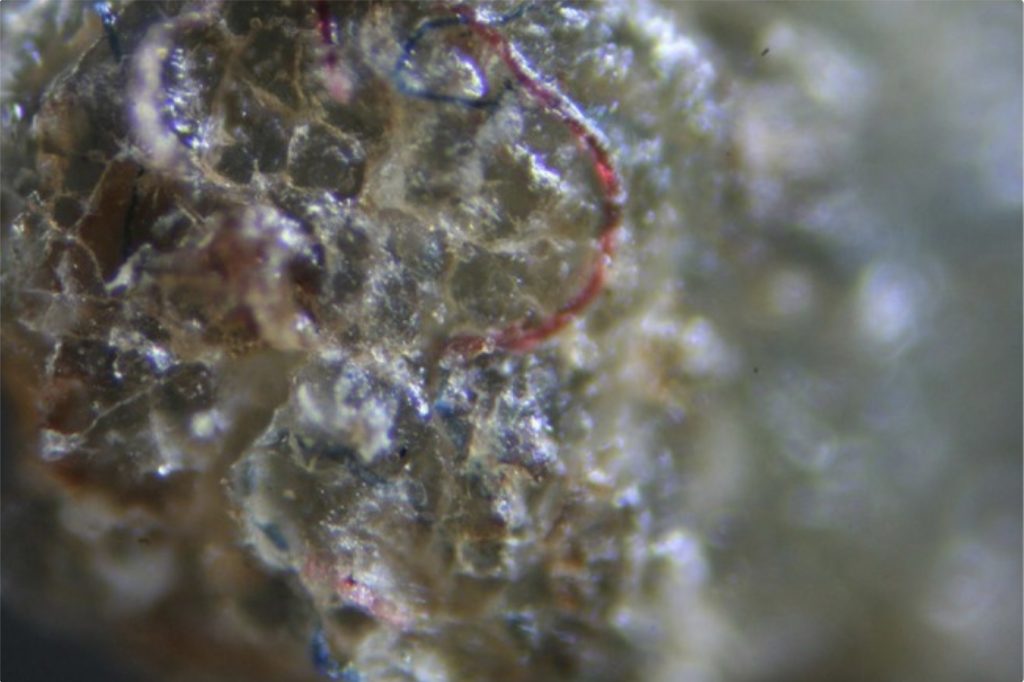
There are even forms of Lyme disease where people can get fibers coming out of their skin, known as Morgellon’s disease. This can cause painful, ulcerating skin lesions, as noted below:
Images courtesy of: Middelveen MJ, Stricker RB. Morgellons disease: a filamentous borrelial dermatitis. Int J Gen Med. 2016 Oct 14;9:349-354. doi: 10.2147/IJGM.S116608. PMID: 27789971; PMCID: PMC5072536.
If you get a tick bite in Europe, the rashes can be different than the American varieties. A strain of Borrelia (Borrelia afzelii) can cause a reddish/violaceous skin rash, usually of the hands or feet, known as ACA (Acrodermatitis chronicum atrophicans)—it’s the European version of our EM rash. I have seen it in patients who lived in Europe and returned to the US, although we are now finding this species of Borrelia in ticks here in the States. See below:
Images courtesy of: https://dermnetnz.org/topics/acrodermatitis-chronica-atrophicans
Acrodermatitis chronica atrophicans: Dr Daniela Vanousova, Dermatologist, Czech Republic; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, July 2015. DermNet NZ Revision October 2021
Occasionally, Borrelia spp. will also cause hard, reddish nodules on the earlobes, nipples, and/or scrotum in children called Borrelia lymphocytomas.
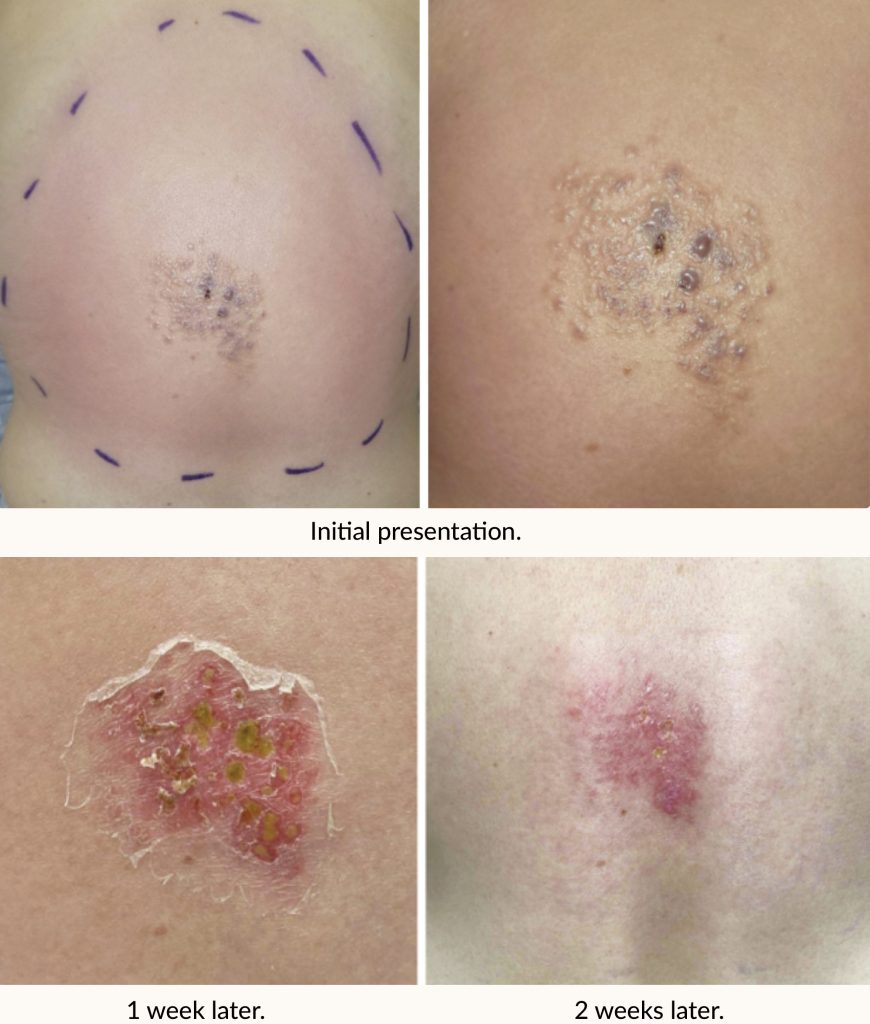
These images show different skin manifestations of Borrelia. You can see why it’s called the Great Imitator–and why vigilance is a must.
[Images courtesy of: Zhang ZZ, Hashemi DA, Kroshinsky D. Disseminated Lyme disease with a herpetiform center. JAAD Case Rep. 2022 Mar 12;29:46-47. doi: 10.1016/j.jdcr.2022.02.034. PMID: 36193244; PMCID: PMC9525727.]
[Images courtesy of: Myszkowska-Torz A, Tomaszewski M, Kotowski M, Witczak C, Figlerowicz M, Mazur-Melewska K. Cutaneous Manifestations of Lyme Borreliosis in Children-A Case Series and Review. Life (Basel). 2022 Dec 27;13(1):72. doi: 10.3390/life13010072. PMID: 36676022; PMCID: PMC9864164.]
The above EM rashes are proof of exposure to Lyme disease and do not require a blood test for confirmation. However, due to the wide range of potential skin rashes, if you have an atypical EM rash, proper identification requires seeing a Lyme-literate healthcare provider as well as a dermatologist who may do a biopsy to differentiate the rash from other causes.
Lyme rashes will slowly disappear over time whether you treat them with antibiotics or not, but without treatment the infection itself will eventually develop into a chronic form of the disease with the debilitating symptoms you already know about.
And, of course, if you never develop a rash but are still infected, you will need blood tests for confirmation.
This is part one of a two-part series originally published on Substack by Dr. Richard Horowitz. You can read the second part, Let’s Talk About Testing for Lyme Disease, Part 2 – Blood Tests, next time.
See also:
“Medical Detective” series brings information you need to know
MEDICAL DETECTIVE #1: An overview of Lyme disease signs and symptoms
MEDICAL DETECTIVE #2: How Will I Know If I Have Lyme Disease?
Dr. Richard Horowitz has treated 13,000 Lyme and tick-borne disease patients over the last 40 years and is the best-selling author of How Can I Get Better? and Why Can’t I Get Better? You can subscribe to read more of his work on Substack or join his Lyme-based newsletter for regular insights, tips, and advice.
























We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page