MEDICAL DETECTIVE: Establishing the diagnosis of Bartonella
This article was originally posted on Dr. Richard Horowitz’s Medical Detective Substack. It is Part 2 of a 5-part series. You can find more helpful content by subscribing here.
By Dr. Richard Horowitz
As you learned last week in Bartonella Part 1, this is a very tricky bacteria, with symptoms overlapping many of those associated with chronic Lyme disease and other co-infections.
Since there are so many species of Bartonella, the first step is to determine if Bartonella is actually in your body. As a Medical Detective, I know that there are certain clues to follow, but what exactly are they?
Clues to the Existence of Lyme and Bartonella in Chronic Illness
Let’s start at the beginning. You’ve been diagnosed with chronic Lyme disease–you had a prior EM rash and/or filled out the questionnaire and scored above 63, implying a high likelihood of exposure. See the prior Medical Detective Substacks on using this HMQ questionnaire:
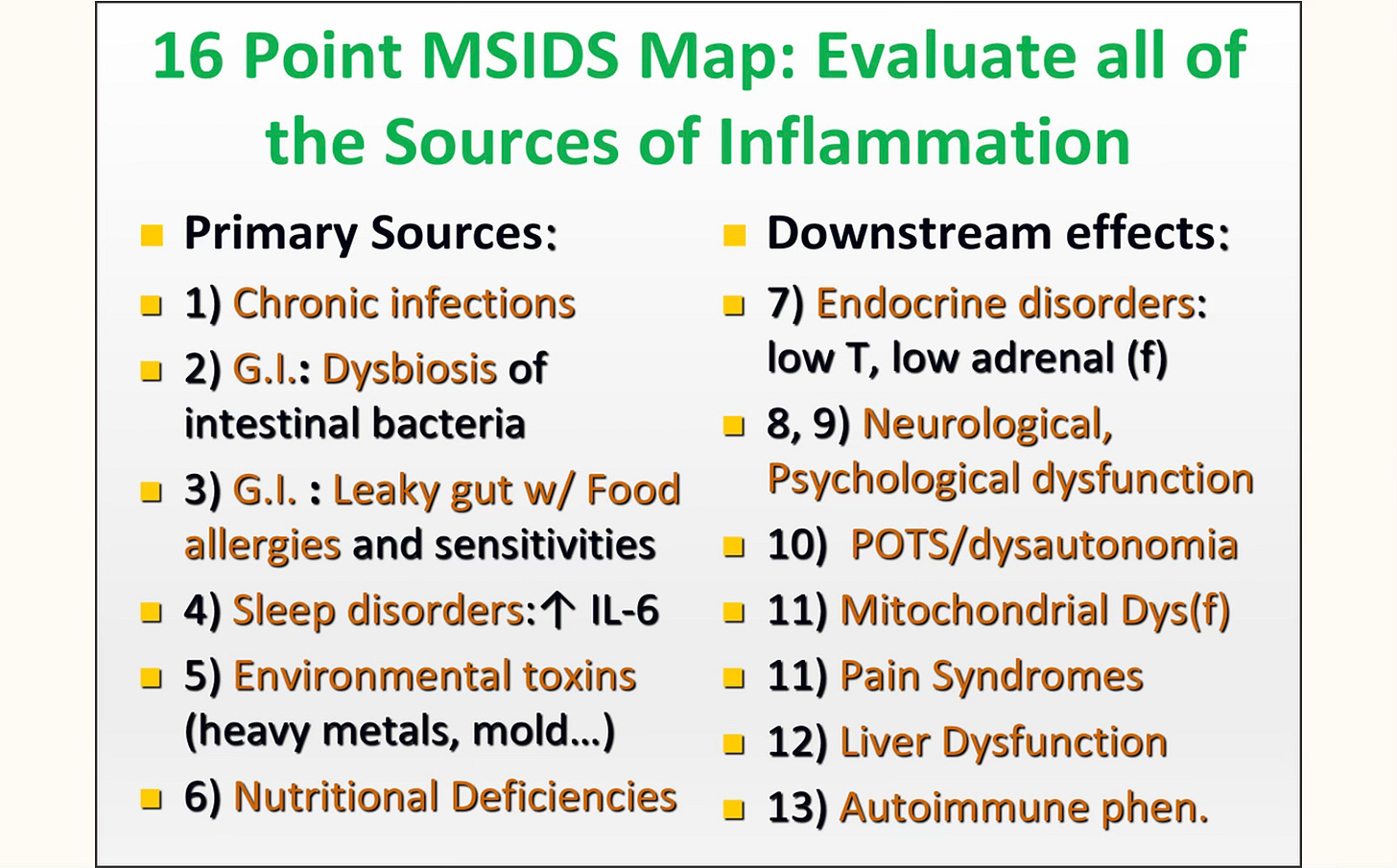
Remember, however, you can have up to 16 different reasons why you’re still ill. This is, as you know, what I call the multifactorial diagnostic and treatment model MSIDS. It is important to keep going back to this model, because there can be multiple causes of overlapping inflammation causing the same symptoms:
.
Diagnosing Chronic Lyme Disease with 6 Key Clinical Features and Laboratory Values—and How This Relates to Bartonella
Go back to the Medical Detective Substacks from July 2024 (starting with this one) for all the details you’ll need. For now, I can summarize the factors that lead to a diagnosis of Lyme disease:
You not only have a significant score on the HMQ, but have up to six key clinical features of Lyme disease:
- A multisystemic illness is present. Although you might just have one swollen joint, most people have a multisystemic illness, with fatigue, pain, headaches, memory/concentration problems, mood disorders, and insomnia with different body systems affected. This is also the case with Bartonella.
- Symptoms come and go with good and bad days without another explanation.
- You have migratory pain in your joints, and/or muscles, and/or nerves, a key clinical feature of both acute and chronic Lyme disease. (FYI, there are only seven diseases causing migratory pain: acute rheumatic fever, acute hepatitis, inflammatory bowel disease, gonococcal arthritis, Reiter’s syndrome, lupus, and chronic Lyme disease. See prior Medical Detective Substacks on symptoms/testing to rule these out.).
- Women tend to have increased symptoms right before, during, or after their periods, due to low estrogen levels bringing out symptoms.
- Antibiotic therapy makes symptoms better or worse. Improved symptoms are due to lowering down the load of the bacteria increasing inflammation; an increase is be due to a Jarisch-Herxheimer reaction, killing off bacteria with inflammatory cytokine release. This is also the case with Bartonella.
- Laboratory testing is positive for Lyme disease and/or Bartonella.
The July 2024 Medical Detective Substacks discussed in detail that tests for TBDs are not reliable (ELISA, Western blot) due to the many different strains of Borrelia found all over the world making people really ill.
Why is it so important to know everything you can about Lyme disease? Because once you have established a diagnosis of Lyme, not only is it highly likely you will find Bartonella associated with a Borrelia infection, but the treatment for chronic Bartonella, like chronic Lyme disease, involves using dapsone combination therapy in our medical practice.
Although many different healthcare providers use different treatment regimens, my goal has been to find the shortest, most effective oral, generic antibiotic combo for the treatment of Bartonella, and to date, we have published the only one that involves short term antibiotic pulses. (I’ll discuss this in upcoming Substacks
Lyme disease can oftentimes be effectively treated with a nine-week double dose dapsone combination therapy (DDDCT) followed by a four-day high dose dapsone pulse (HDDCT), but Bartonella requires not only this treatment for CLD, but multiple two-week HDDCT pulses, 6-8 weeks apart, with six days of HDDCT.
So the treatments are similar (they are both biofilm/persister bacteria), but Bartonella is a much more fastidious bacteria requiring multiple pulsed biofilm/persister drug regimens to knock down the load of the bugs. And the more MSIDS factors causing inflammation (like mold toxicity), the more pulses may be required.
Clues that You Might Have Bartonella Once You Have Established a Lyme Diagnosis
Clue #1: Testing
Go back to last week’s Substack, Bartonella Part 1, to read about the three levels of testing.
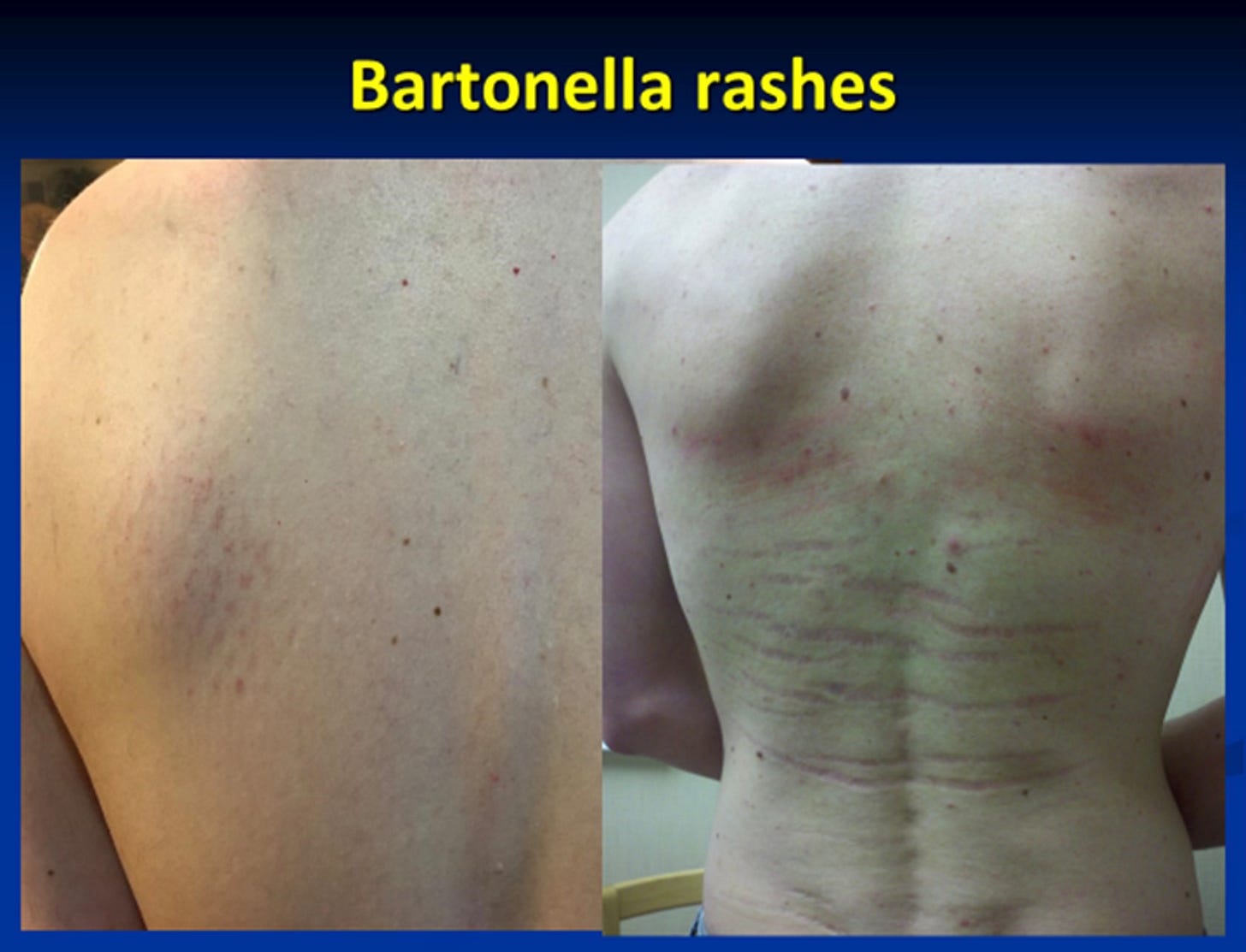
Clue #2: A Rash
If you have a rash, just as an EM rash is pathognomonic for Lyme disease, the classical Bartonella rashes show that you’ve been exposed to a Bartonella species.
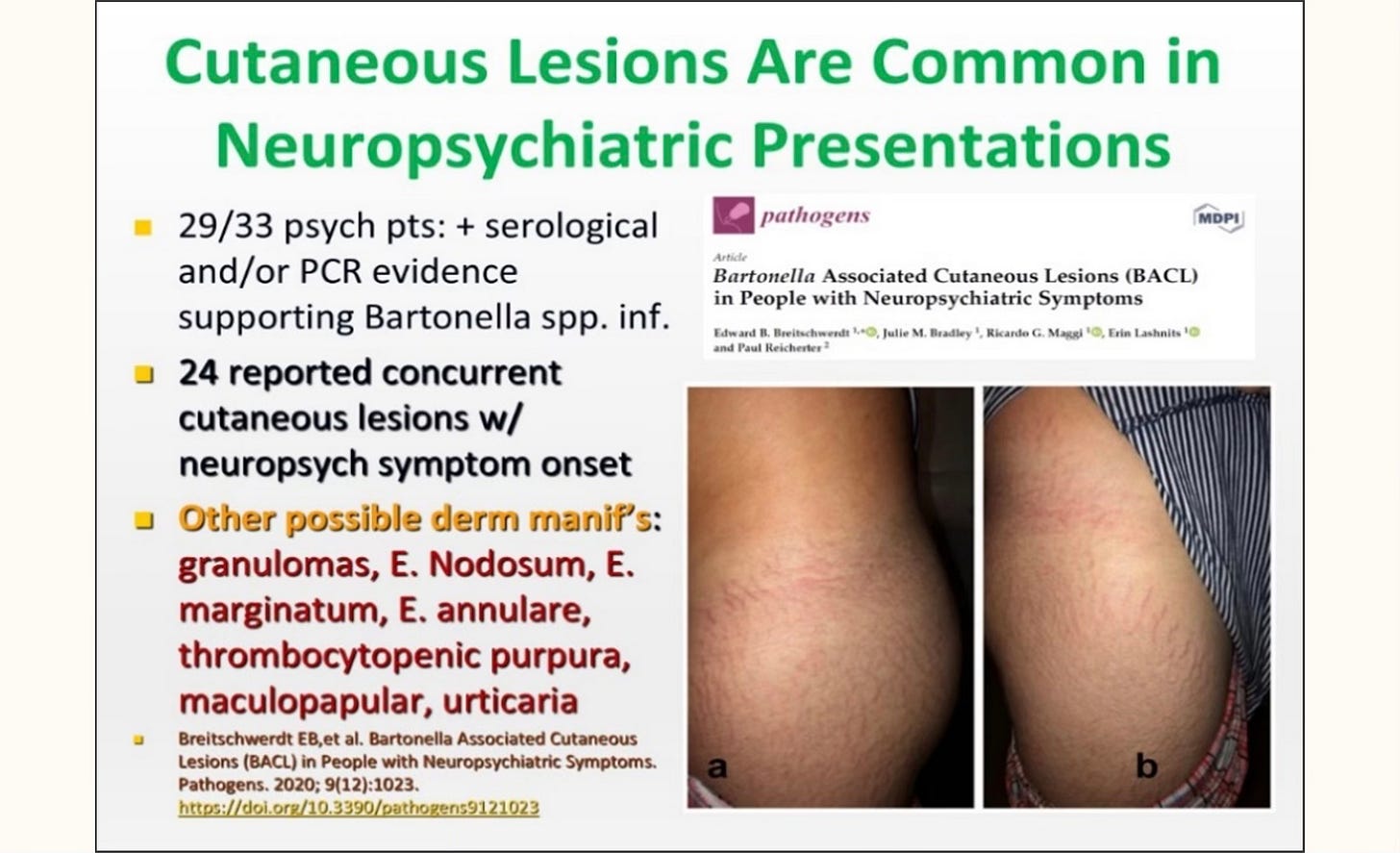
[From: Breitswerdt E et al, Bartonella associated cutaneous lesions (BACL) in People with Neuropsychiatric Symptoms. Pathogens 2020; 9(12):1023]
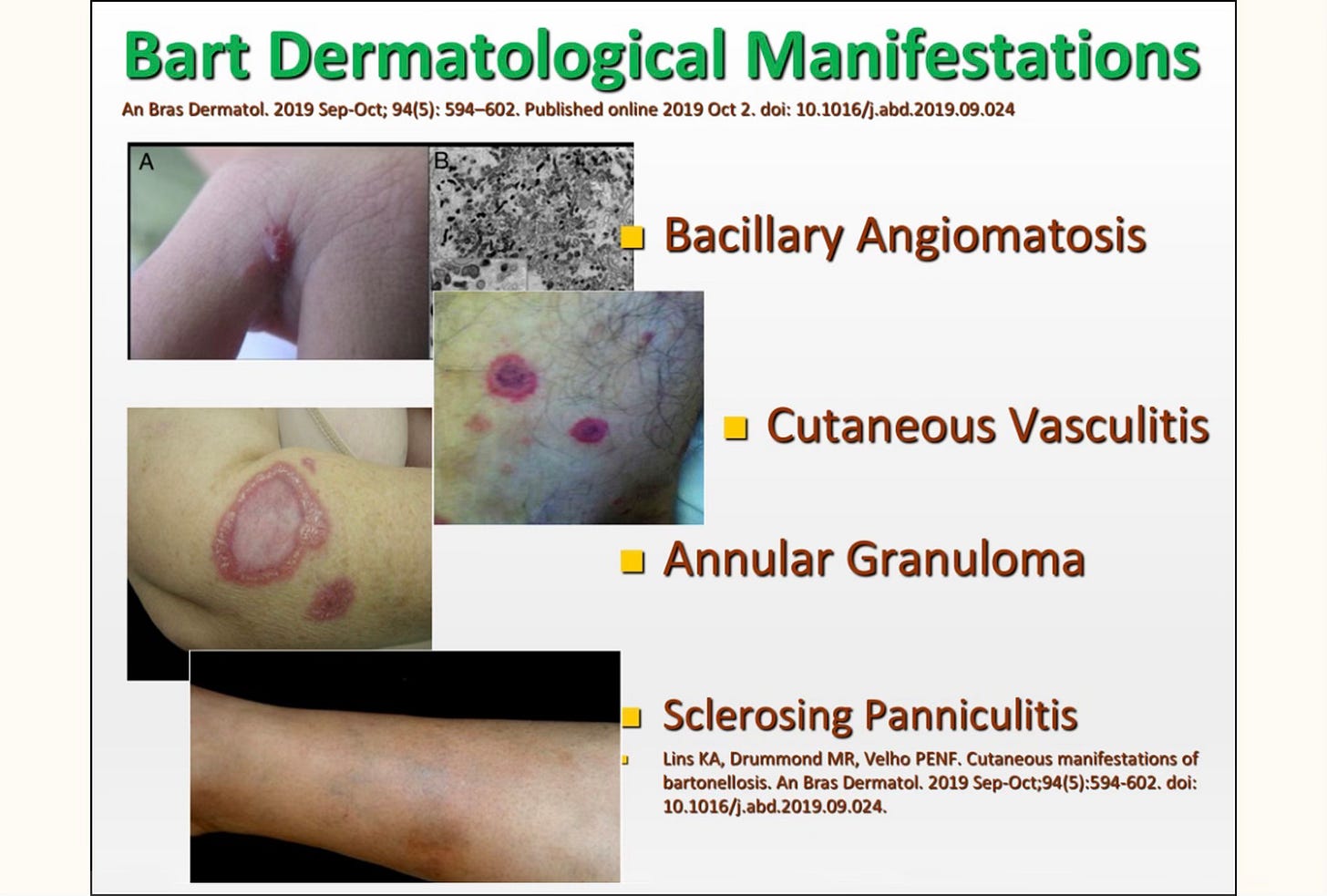
[From: A Bras Dermatol. 2019 Sep-Oct; 94(5): 594–602. Published online 2019 Oct 2. doi: 10.1016/j.abd.2019.09.024]
These rashes that look like ‘stretch marks’ (striae) may have a dark red appearance and look like a Christmas tree pattern (see below) or be perpendicular to the skin planes, but oftentimes we see white striae instead, over the hips, thighs, lower back, breasts, upper chest…and they may change color over time.

Clue #3: Other Symptoms
Bartonella exposure usually results in a worsening of underlying Lyme symptoms, with several key clinical symptoms:
Other Symptom Clue #1: Severe Neuropathy
Patients with underlying Bartonella had severe neuropathic symptoms, including severe pain on the bottom of their feet as well as severe neuropathy of the hands, feet (tingling, burning, numbness, stabbing sensations) that was resistant to standard neuropathic medication like gabapentin, duloxetine, amitriptyline, and/or pregabalin. Some patients had Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) with or without small fiber neuropathy.
Other Symptom Clue #2: Severe Autonomic Neuropathy
Patients with multiple Bartonella species were the ones with the worst POTS (Postural Orthostatic Tachycardia Syndrome). They would stand up and feel like they were going to pass out (pre-syncope), pass out (syncope), and have severe overlapping fatigue, palpitations, anxiety and brain fog. They were oftentimes needing POTS medication apart from extra salt and fluids, like midodrine, fludrocortisone, and/or droxidopa.
Other Symptom Clue #3: Immune Deficiency
When multiple Bartonella species were present, we often found chronic variable immune deficiency (CVID) with low immunoglobulin levels and/or low Immunoglobulin subclasses.
Other Symptom Clue #4: Severe Neuropsychiatric Presentations
These patients often had severe anxiety, depression, OCD, bipolar disorder, and/or schizophrenia which was resistant to standard medication.
Other Symptom Clue #5: Severe Eye Problems, New Onset of a Seizure Disorder, Large Unexplained Lymph Nodes
Bartonella has a propensity to invade the Central Nervous System and cause eye inflammation (conjunctivitis, uveitis, optic neuritis, retinal and arterial occlusions); a new, unexplained seizure disorder; and/or large lymph nodes, resembling other medical diseases like sarcoidosis.
The species of Babesia and Bartonella that were found in those patients who had the worst clinical symptoms (see Table 4 in our published article) included evidence of exposure to B. microti, B. duncani, B. divergens, B. odocoilei, and multiple species of Bartonella, including B. henselae, B. quintana, B. elizabethae, B. vinsonii subspp., B. koehlerae, and B. bacilliformis.
Now that You Have a Diagnosis, What Are the Next Steps for Treatment?
If you have done an MSIDS review, as discussed above, and discovered overlapping causes of inflammation, you have to decide whether these may/will interfere with the success of DDDCT (double dose dapsone combination therapy) and HDDCT (high dose dapsone combination therapy) for the treatment of chronic Bartonella.
The most common examples are overlapping infections with Babesia, a malarial-like parasite; long COVID; and mold toxicity; although other factors like POTS/dysautonomia, low adrenal function, etc. will all interfere with clinical success. You can see how many factors we found in those suffering from bartonellosis and chronic Lyme disease:
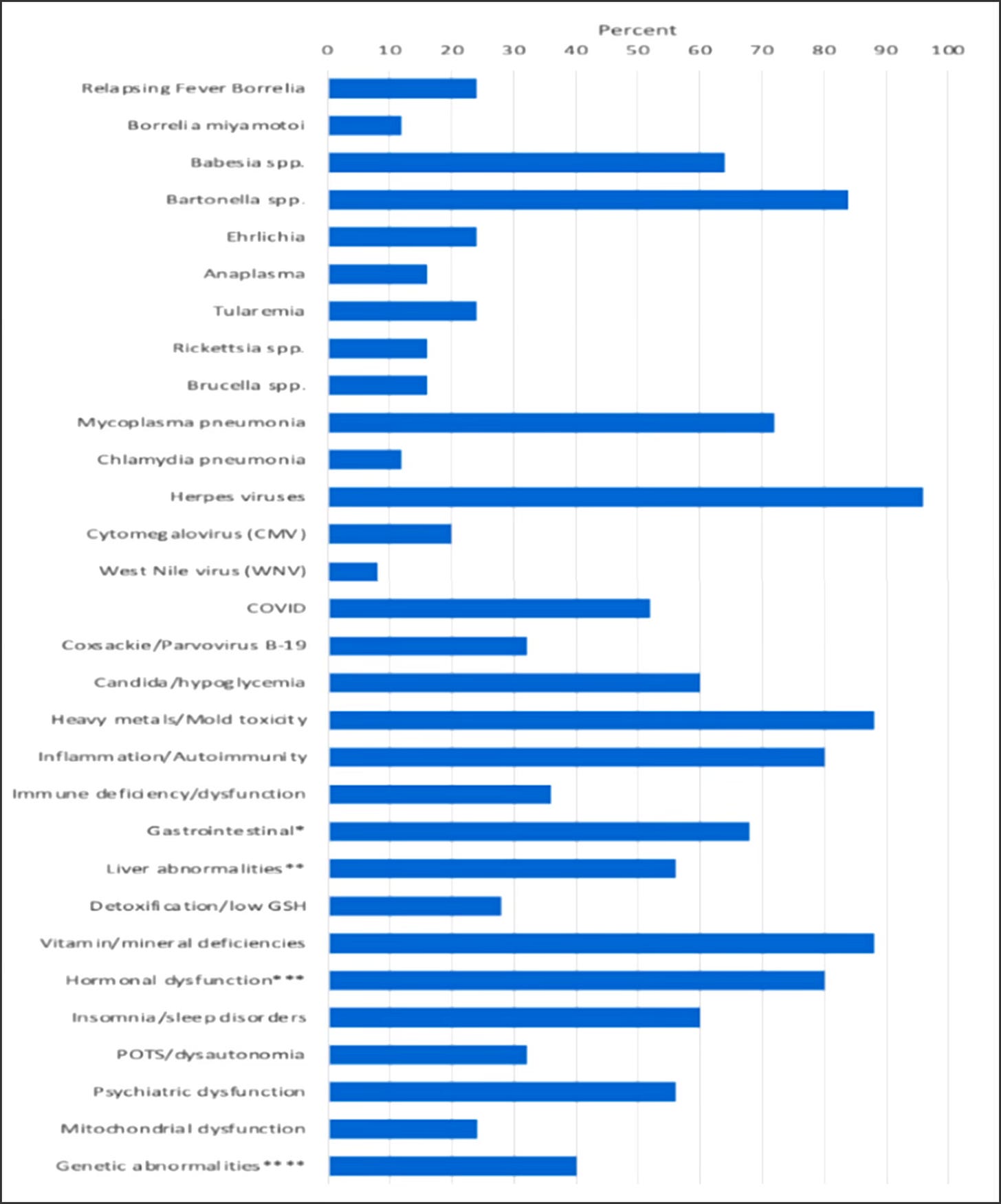
[From: Horowitz, R.I.; Fallon, J.; Freeman, P.R. Comparison of the Efficacy of Longer versus Shorter Pulsed High Dose Dapsone Combination Therapy in the Treatment of Chronic Lyme Disease/Post Treatment Lyme Disease Syndrome with Bartonellosis and Associated Coinfections. Microorganisms 2023, 11, 2301. https://doi.org/10.3390/microorganisms11092301]
Bartonella is a biofilm, persister bacteria, as is Lyme disease, so I usually will start with the 8–9-week oral, generic dapsone combination protocol.
But in the meantime, you need to ensure that there has been a comprehensive evaluation of all factors causing chronic illness. For example, if you have gastrointestinal issues and/or detoxification issues, these may need to be addressed first to ensure tolerance of the protocol.
Remember, Bartonella Can Be Just One of the Reasons Why You’re Chronically Ill
It is not enough to just find Bartonella and/or Lyme and treat it with antibiotics. The rule of thumb with the MSIDS map is to determine all overlapping factors keeping you ill:
*Evaluate other underlying infections (bacteria, viruses, parasites, fungi), which is #1 on the MSIDS model driving the chronic disease process. Co-infections often increase underlying symptoms, making them resistant.
Babesia makes Lyme patients much sicker and will interfere with the full success of DDDCT and HDDCT treatment for Bartonella and Lyme. (Fevers, chills, day sweats, night sweats, flushing, unexplained air hunger, and a cough are classical symptoms of Babesia.)
Co-infections can also increase neurological symptoms; As discussed above, was there a new onset of a seizure disorder, eye problems (retinitis, uveitis), severe neuropathy, POTS with or without neuropsychiatric problems, and/or immune deficiency indicative of overlapping Bartonella?
Remember that most ticks are now co-infected with many species, so there can multiple overlapping co-infections all at once making you ill. In 2021, French researchers, found a shocking 16 different possible infections in patients with multiple symptoms likely related to a tick bite. Of these, 48% were co-infected, with 25% having exposure to at least three organisms.
From: Lacout A, Mas M, Pajaud J, Perronne V, Lequette Y, Franck M, Perronne C. Real time micro-organisms PCR in 104 patients with polymorphic signs and symptoms that may be related to a tick bite. Eur J Microbiol Immunol (Bp). 2021 Nov 3;11(3):62–75. doi: 10.1556/1886.2021.00011.
Key Facts
So when beginning your journey of diagnosing and treating Bartonella, remember key facts:
- Evaluate environmental factors (toxins like heavy metals, mold, pesticides). I’m finding mold toxins in the vast majority of my patients, and this can interfere with the success of DDDCT and HDDCT, so consider testing early on with a RealTime Laboratory mycotoxin urine test, and if positive, nasal swab for biofilms and mold spores.
- Evaluate genetic factors (HLA status, autoimmune markers, SNPs, detoxification pathways).
- Evaluate other overlapping sources of inflammation (leaky gut, food allergies, mineral deficiencies, insomnia, PTSD).
- Evaluate downstream effects of inflammation (hormonal dysregulation, with low adrenal function, sex hormones or thyroid deficiency; ANS dysfunction with POTS; liver inflammation, mitochondrial damage)
Before moving on to just treating Bartonella and/or CLD/PTLDS and Bartonella, make sure that all other co-infections have been evaluated, as well as important MSIDS variables like mold and long COVID that can cause similar symptoms.
Otherwise you will find yourself wondering why the treatments are not as effective as you would expect. In my next installment, you’ll read all about dapsone combination therapy, an effective treatment for both chronic Lyme disease and Bartonella.
Dr. Richard Horowitz has treated 13,000 Lyme and tick-borne disease patients over the last 40 years and is the best-selling author of How Can I Get Better? and Why Can’t I Get Better? You can subscribe to read more of his work on Substack or join his Lyme-based newsletter for regular insights, tips, and advice.




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page