LYMESCI: Ehrlichiosis — The Tick-Borne Disease No One Has Heard Of

According to the experts, ticks and the diseases they carry are expanding into new geographic areas. While the majority of Americans have heard of Lyme disease, fewer than 2% have any knowledge of another tick-borne disease called ehrlichiosis. (1, 2)
As a matter of fact, my own child was CDC positive for an Ehrlichial infection (amongst other things), and when I took her to the Emergency Room for an irregular heartbeat that developed during treatment, the ER doctor told me he had never heard of “Ehrlichia chaffeensis.” True story!
Warning! Ehrlichiosis Infections
In May 2017, an article in the CDC “Emerging Infectious Diseases” Journal, warns that ehrlichiosis infections are being “grossly underreported” in the U.S. with as many as 97-99% of infections going unrecognized. They are projecting that the actual number of annual cases could go as high as 1/2 the number of Lyme disease cases—which would mean we may already have over 150,000 cases of ehrlichiosis annually. (3)
There are several factors causing the underreporting:
- Lack of public education/knowledge—doctors aren’t testing for or diagnosing ehrlichiosis.
- Some cases are mild enough that patients do not seek medical care or a diagnosis.
- Insensitive or inaccurate testing methods may result in false-negative diagnosis.
- Reporting is voluntary and the criteria are restrictive.
Ehrlichosis Tick-Borne Diseases
Ehrlichiosis is the name for several tick-borne diseases that are caused by a group of bacteria known as Ehrlichia. Ehrlichia belong to a larger order of bacterium known as Rickettsiales. (4) (See my previous post on the spotted fever group of Rickettsiae)
Rickettsiae and Ehrlichia belong to a broad group of bacteria that can be spread by a tick bite. These infections can be transmitted alone or at the same time as Lyme disease and are commonly known as co-infections. (I talk more about co-infections here)
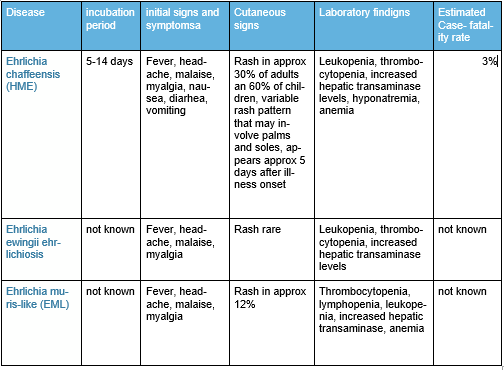
The Ehrlichia (E) group includes: (5, 6, 7, 8,)
- chaffeensis: the cause of human monocytic ehrlichiosis (HME)
- ewingii
- muris-like (EML)
Ehrlichiosis Symptoms
While some cases of ehrlichiosis are mild, the disease can be severe or fatal if not treated correctly, even in previously healthy people. Severe symptoms of ehrlichiosis may include difficulty breathing, respiratory failure, bleeding disorders, kidney or heart failure.
Because Ehrlichia infect white blood cells (the cells that fight infection), and mitochondria (the powerhouse of the human cell) the consequences of untreated infection may have long-lasting effects.(9) I often wonder if undiagnosed Ehrlichiosis isn’t responsible for some portion of the millions of people with the mysterious illness known as “Myalgic Encephalomyelitis” or “Chronic Fatigue Syndrome”.
Other symptoms of ehrlichiosis can include:
- Fever/chills and headache (majority of cases)
- Fatigue/malaise (over two-thirds of cases)
- Muscle/joint pain (25% – 50%)
- Nausea, vomiting and/or diarrhea (25% – 50%)
- Cough (25% – 50%)
- Confusion or brain fog (50% of children, less common in adults)
- Lymphadenopathy (47% – 56% of children, less common in adults)
- Red eyes (occasionally)
- Rash (approximately 60% of children and 30% of adults)
Ehrlichiosis Diagnosis and Treatment
Like other tick-borne diseases, diagnostic blood tests will frequently be false-negative during the first weeks of illness. And like other tick-borne diseases, treatment is most effective if started early. For this reason, healthcare providers must use their best clinical judgement and treat patients based upon early symptoms alone.
According to the CDC website: “The diagnosis of ehrlichiosis must be made based on clinical signs and symptoms, and can later be confirmed using specialized confirmatory laboratory tests. Treatment should never be delayed pending the receipt of laboratory test results, or be withheld on the basis of an initial negative laboratory result.”
The CDC goes on to say: “Doxycycline is the first line treatment. for adults and children of all ages and should be initiated immediately whenever ehrlichiosis is suspected.” >(10)
Patients who are treated early may recover quickly on outpatient medication, while those who experience a more severe illness may require intravenous antibiotics, prolonged hospitalization or intensive care.
Ehrlichiosis Transmission
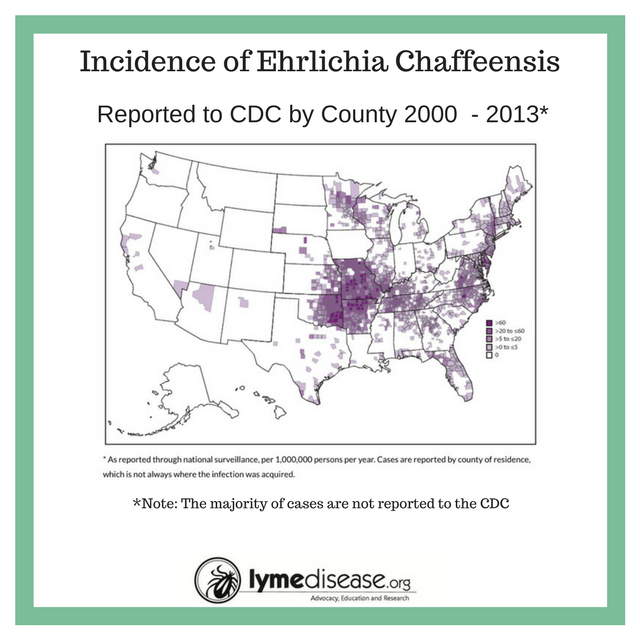
The lone star tick (Amblyomma americanum) is the primary vector of E. chaffeensis (HME), and E ewingii with rates of infection ranging from 0 to 27 percent. In the past decade the lone star tick has expanded into geographic areas where it did not previously occur. This is particularly concerning because the lone star tick is an aggressive biter.
Ehrlichia bacteria have been found in other ticks including the Pacific Coast tick (Ixodes pacificus), Gulf Coast tick (Amblyommma maculatum), American dog tick (Dermacentor veriabillis), and the brown dog tick (Rhipicephalus sanguineus), but there is not a lot of research into how effectively these ticks are able to transmit Ehrlichia to humans. (11, 12)
Preliminary studies suggest that the vector for the newest species E. muris-like (EML) found in Wisconsin and Minnesota is the deer tick (Ixodes scapularis), and in a recent publication, researchers found that 40% of Pacific Coast ticks were carrying three different types of Rickettsia bacteria. (8, 13)
While there is some geographic overlap, in general these ticks are found in the following areas:
- Lone star tick (east of the Rockies)
- Gulf Coast tick (Gulf and Southern states)
- American dog tick (east of the Mississippi)
- Blacklegged or “deer” tick (east of the Rockies)
- Western blacklegged tick (west of the Rockies)
Other modes of transmission
Ehrlichia chaffeensis has been shown to survive for over a week in refrigerated blood. Therefore these bacteria may present a risk for transmission through blood transfusion and organ donation. It has also been suggested that ehrlichiosis can be transmitted from mother to child, and through direct contact with slaughtered deer. (14, 15)
Summary of Ehrlichiosis
In my next post, I will address another type of rickettsial illness: Anaplasmosis
References:
- CDC | Emerging Tickborne Diseases | Public Health Grand Rounds, March 2017
- U.S. public’s experience with ticks and tick-borne diseases: Results from national HealthStyles surveys
- Relative Risk for Ehrlichiosis and Lyme Disease in an Area Where Vectors for Both Are Sympatric, New Jersey, USA
- CDC MMWR | Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis — United States, May 2016.
- Human infection with Ehrlichia canis, a leukocytic rickettsia, 1987.
- Ehrlichia chaffeensis: a Prototypical Emerging Pathogen, 2003.
- Tick-borne ehrlichiosis infection in human beings, 2008.
- Emergence of a new pathogenic Ehrlichia species, Wisconsin and Minnesota, 2009.
- Ehrlichia’s molecular tricks to manipulate their host cells, 2015.
- CDC: Ehlichiosis
- Natural history of Ehrlichia chaffeensis: vertebrate hosts and tick vectors from the United States and evidence for endemic transmission in other countries, 2010.
- Survey of Ixodes pacificus Ticks in California Reveals a Diversity of Microorganisms and a Novel and Widespread Anaplasmataceae Species
- Species composition and temporal distribution of adult ixodid ticks and prevalence of Borrelia burgdorferi sensu lato and Rickettsia species in Orange County, California
- Perinatal Transmission of the Agent of Human Granulocytic Ehrlichiosis
15. Exposure to deer blood may be a cause of human granulocytic ehrlichiosis




















Excellent article. Please remember that a person can be bitten and contract the same disease/s multiple times. Since these diseases are bacterial, a person does not become immune to them after having the disease once. They must be re-tested when symptomatic to access for the need for another treatment, for the same disease and/or others.
I’ve been battling ehrlichiosis for at least a month now. I suspect that I’ve had it for several months , but didn’t suspect a tick-bite as the cause for my problems.
It’s now late June. Sometime a few months ago (approximately late fall) I developed an itchy bump in my upper right butt crack. I occasionally had some fever and mental disorientation, but it would come and go. I had some diarrhea and nausea, and figured I had some kind of stomach flu. I thought I’d get over it on my own, and didn’t seek medical treatment. No big deal.
In early spring I was doing some yard work here and received a tick bite on my lower back. I pulled the tick out, but apparently the head broke off and became lodged under my skin. It developed a painless lump. There was no rash or discoloration, so I didn’t think much of it. Not long after this, I started having severe stomach and intestinal irritation, which soon turned into nausea, vomiting, dry-heaving, throwing up bile and diarrhea. I felt mentally disoriented and dizzy, tingly in the head and body. I had severe vertigo and lethargy.
I decided to seek medical help at this point. They did a blood test on me and didn’t find a high white blood cell count or any antibodies in my system against heliobacter pylori, so they diagnosed me with GIRD and gave me stomach medication.
At this point I didn’t suspect the tick bite on my back as the source of my illness, so I didn’t report it to my doctor. My body fought off the disease on its own. One day when I suddenly started feeling better, I reached back and discovered that the lump under my skin was suddenly gone. I connected the dots and went back in to the doctor for a follow-up evaluation. I told them that I now suspected a tick-borne disease. They did another blood test, this time testing for tick disease and I tested positive for ehrlichiosis. They put me on doxycycline. Not only did the lump on my back disappear,but so did the itchy bump in my butt crack. I’m still on the antibiotic until next Sunday. It makes me feel kind of sick too, but I’ll endure this to get rid of the tick disease!
I guess I’m lucky that I didn’t have more severe symptoms and that I found the culprit. It could have been worse. I can’t wait to get off of the antibiotics and start feeling good again. I’ve learned to always wear insect repellent when in the woods and not to take seemingly benign lumps under my skin lightly.
My husband was in hospital 14 days with Ehrilichiosis. He has Parkinson’s so he got a double whammy. Spiking fever, lost at least 20 lbs. was on a walker, speech difficulty. This is a dangerous tick. and it was found in TN.
I ended up in the hospital with this in July, 2017. I had a tick bite 2 weeks prior, but since I didn’t see any rash (bullseye rash) I assumed I was clear from the tick bite. I had never heard of ehrlichiosis and apparently, other medical professionals hadn’t either. I was first diagnosed with a sinus infection because I was spiking 104 temps with severe headaches for a week prior to hospitalization. When I went to the ER, they attempted to do a lumbar puncture and failed after 3 attempts, finally getting it right the next day after admission. At this point, I did tell everyone that I had a tick bite 2 weeks prior, but they were more interested in meningitis. After a negative CT scan of my head, they admitted me and tried (i believe) 2 other IV antibiotics at this point while I was in a room on isolation. I just got worse, and one after another, doctors came into the room to inform me that I had leukopenia, thrombocytopenia, elevated liver enzymes, mild congestive heart failure, and abnormal heart rhythm. Only one doctor related all this to a tick bite, the others were just focused on the symptoms and made it seem that these symptoms were all unrelated and I had been walking around with a bad heart. Despite my age, I kept telling them that I routinely ran, did high intensity aerobic exercise, and had no prior problems. They acted as they didn’t believe me. I got worse the first 2 days with extreme confusion, could barely write my name, and couldn’t sleep because of joint pain, I even became urinary incontinent.
They finally started me on the doxycycline after 2 days and the fever abated. I was allowed to leave the hospital after 5 days with a discharge diagnosis of viral meningitis and no real understanding of what it was I had. I tried to go back to work, but people would look at me and then tell me how bad I looked (I lost 20lbs.) I couldn’t make a full day, nor could I resume exercising. I felt horrible and I knew that if it was viral meningitis, I should have felt better after a week, but I didn’t. Doing my own research online, I found the CDC description of ehrlichiosis and the symptoms matched exactly what I had experienced. One week after discharge, I went to my primary who did an office EKG on me and it showed my heart in normal sinus rhythm. All the the medication they stuck me on because of my heart irregularities were just making things worse and I stopped taking them. When I went to the infectious disease doctor for a 2 week follow-up, he finally told me what I had, but I stole his thunder by telling him that I already knew.
The bottom line is I feel that they could have gone by the symptoms and started me on the right antibiotic sooner at the hospital. I had already delayed treatment a week by going under the assumption that I had a sinus infection. I was contacted by the health department after discharge, since this was a reportable disease, and the woman I spoke with was infinitely more knowledgeable about the disease and gave me more valuable information than all those doctors. She recommended that I do another course of the antibiotic because they had only prescribed a 10 day course and I was starting to have symptoms of relapse after finishing it. I did, and today I am back to my usual activities. On the Florida Disease Frequency Report, I am one of two reported cases so far this year for my county. I read of an earlier case similar to mine of a gentleman about 8 years older than me who got a tick while visiting a Florida State Park. Like me, when he got sick, he was treated for a sinus infection. Eventually, like me, he ended up at the ER. They apparently didn’t know how to respond to his symptoms and this gentleman died in the ICU a week later. They really need to let people know that there is more than Lyme’s disease out there and just because you didn’t get a bullseye rash, doesn’t mean you’re in the clear. Doctors need to act immediately on symptoms presented if a tick was reported in the process and all immediate tests come up negative for other factors. They could most certainly do a better job of informing the patient what to expect with this stuff and be more reassuring than just marching into the room to list off a dire list of symptoms and then walk off with no explanation. I had one doctor who did relate all the symptoms as possibly tick related and that helped me immensely on dealing with it.
It’s been six months since I was in the hospital with pneumonia caused by Ehrlichia and I’m suffering from sore, achy muscles daily along with fatigue . Does anyone know if this is s lifetime sentence of this tick disease?
This disease nearly finished me. What follows is my close recollection, though it’s been over 10 years now.
Back in 2005 – a healthy 30 something – I began to have a horrible headache, body aches, flu-like joint pains and a low grade fever.
The thing was, this headache, along with the fever, persisted for days and days. NOTHING I took would help. I was a hardheaded younger man and let this continue for probably well over a week like this.
I went to my PCP and was quickly diagnosed with a sinus infection…given antibiotics and rushed out the door.
Even as I agonized with this headache in his office..telling him this was NOT a sinus infection.
I took the antibiotic for roughly 5 or 6 days – with no noticeable improvement. I’ve noticed I’ve lost 10 or 15 lbs at this point. I’m wrapping a pillow tightly around my head – hoping to get the smallest amount of relief in my darkened bedroom.
So I went back to him. He was “on his way out of the country”, and told me I needed to go to the ER. And so I went.
In agony with this headache, and body aches, a fever around 102 that I can’t kick, I waited in the ER for hours and hours. Even though I’m telling them I’m dying..I’m thinking my head is going to burst – once again, I’m diagnosed with the wrong thing. I can’t even remember what it was now.
They did a ton of bloodwork, I had an MRI or CT scan (I can’t remember which) AND a spinal tap – thinking it was meningitis.
They doped me up with all kinds of things – and after a day – sent me away with some really strong opiate pain medications.
The pain meds actually helped to dull the pain from this excruciatingly insanely painful headache, and the horrible body aches I was having.
But, after a few days something was still not right. At this point I can no longer make it to work, I can’t really leave my bed or move around much. I’m incredibly lethargic, I can’t think or focus.
I actually, literally made peace..told my wife and children, my brother, friends – those things you don’t tell them until you’re really thinking it’s over for you.
I’ve lost about 25lbs at this point, I’m really not functioning well, and my wife runs me to the hospital.
I think I was over 3 weeks into the symptoms of this hellish illness at this point. The ER rushed me right in.
I got incredibly lucky – there just so happened to be a sharp, infectious disease Doctor in the ER at 2:00am. This amazing person – within an hour knew what I was going through, and exactly what was wrong with me based on symptoms, liver and white blood counts and who knows what else.
He brought my wife a printout of this infection – the information from some Medical database.
He told me I was lucky to even be living at this point. Started me on IV doxycycline, which he told me was rare for them to even have, and fed this into me for the next day.
I left the hospital actually feeling the slightest bit better – with stronger pain meds (this doctor actually understood the level of pain I was in), and a long regimine of Doxycyline
.
Within a few days, my State disease center was calling me to verify the doctor’s diagnosis, and gave me a full list of questions about all kinds of things.
It took me at least the next month (off of work as well), to begin to even feel human again. I think it was at least – no kidding – 6 months before I could do much of anything without being absolutely worn out.
I swear that tick took a portion of my life force, part of my soul. I’ve really never felt the same, and as I age, the joint pains get worse, I go though bouts of mental focus issues, and any number of other symptoms, depression and mental heal issues, health issues, etc.
And though it does get better – it took a long time. And I think you never really bounce back if you’ve let the infection go this long.
I truly believe that were it not for my luck in the ER that night, (and shear will for me to live from my wife) I would’ve died the next day.
I’ve never experienced such illness or pain before or since.
I believe there’s a huge lack of understanding of these tick diseases in the very locations where they’re the most prevalent, by most hospitals and doctors.
I also believe there are a whole host of ongoing symptoms, ancillary effects that aren’t documented, and aren’t believed by the medical community as a whole.
This hellish disease took my life from me – and more than that.
I recall having a nasty bite on my ankle – the scar is still there – it had a large white head on it, like a large pimple or boil – itchy. I thought it was a spider bite. Not very uncommon around OK. How I wish I would have had it looked at.
If your head starts REALLY hurting..like you’ve never felt..and you’re running fever..body aches…go demand they check you for tick disease.