Is the CDC going backwards in terms of persistent Lyme disease?

On October 25, 2023, the CDC published a new page on its website entitled Chronic Symptoms Following Infections. It lists “Some disease agents that have been linked to chronic symptoms.” First on that alphabetized list is “Borrelia burgdorferi (bacteria causing Lyme disease).”
Many in the Lyme community, myself included, considered this to be a HUGE leap forward with the CDC finally acknowledging the concept of the chronic symptoms of Lyme disease that are suffered by many.
Unfortunately, on January 12, 2024, the CDC updated a different page on Chronic symptoms and Lyme disease, crushing some of my hopes. That page contains so many errors it almost seems like intentional gaslighting.
While I have witnessed significant positive changes since the inception of the Tick-Borne Disease Working Group, it’s clear we have a long way to go.
Below is a list of just a few of the errors I found on the new “Chronic symptoms and Lyme disease” page.
Post Treatment Lyme Disease Syndrome
Under the subheading “Recommended Terminology,” the CDC states: “The condition where patients experience prolonged symptoms due to Lyme disease is called Post-Treatment Lyme Disease Syndrome (PTLDS) and its cause is currently unknown. The Centers for Disease Control and Prevention (CDC) encourages using this terminology when communicating about prolonged symptoms due to Lyme disease.”
- Here the CDC fails to mention that the term “PTLDS” is a strict research definition that was created to define a subset of patients who receive a prompt diagnosis and treatment for early Lyme disease. Meaning these patients have received 2-4 weeks of antibiotics within one month of the tick bite. PTLDS does not include patients who received a delayed diagnosis—either due to a false-negative Lyme disease test or failure of a physician to recognize the symptoms and give a clinical diagnosis of Lyme disease.
- By using the term PTLDS, the CDC ignores the many patients with late-stage Lyme disease due to a delayed or missed diagnosis. Late-stage, untreated Lyme is by definition a disseminated “chronic” infection, and is much more difficult to treat than early Lyme.
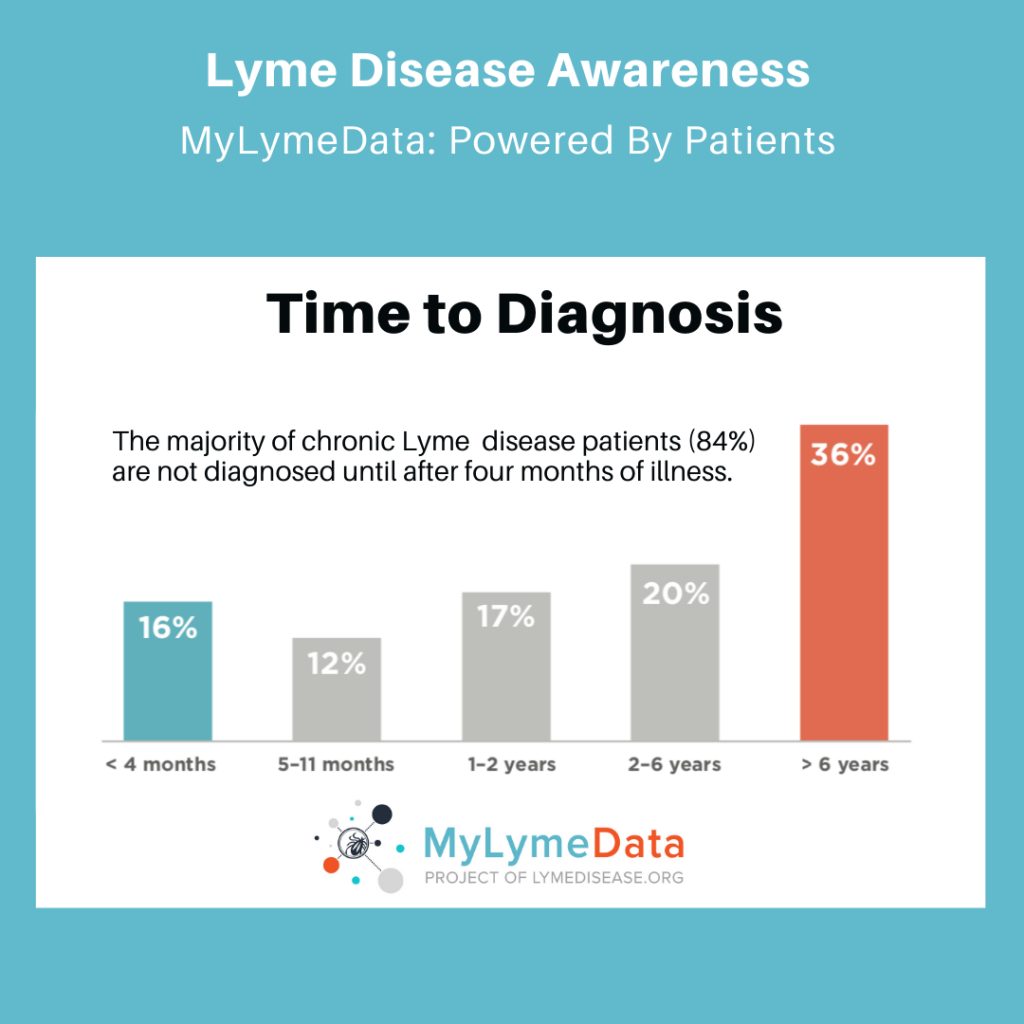
- In LymeDisease.org’s MyLymeData patient registry, now with over 18,000 participants, fewer than 12% of the patients with Lyme disease received a diagnosis within the first month after a tick bite. In fact, over 80% of the participants in MyLymeData with persistent symptoms of Lyme disease were not diagnosed within the first four months of illness.
Prolonged Symptoms
The CDC states: “Lyme disease is an illness caused by the bacteria Borrelia burgdorferi, spread by blacklegged ticks. Although most patients recover completely when treated with a 2- to 4-week course of oral antibiotics, about 5-10% can have prolonged symptoms of fatigue, body aches, or difficulty thinking following treatment.”
- Here the CDC is cherry picking a study that shows only 5-10% of patients with prolonged symptoms after early treatment for Lyme disease. In fact, the most recent study from Johns Hopkins University shows that 14% of PTLDS patients have significant persistent symptoms following prompt treatment for early Lyme disease. (Aucott 2022) An earlier study from Johns Hopkins showed 36% of patients treated for erythema migrans rash (seen in early Lyme) remained ill. (Aucott 2013)
- What the CDC again omits here are the numerous studies showing that a delayed diagnosis and delayed treatment for Lyme disease directly increases the chances of suffering persistent symptoms, with estimates ranging from 26% to 50%. (Johnson 2004)
Chronic Lyme
The “CDC discourages use of the term Chronic Lyme Disease because it implies that prolonged symptoms are caused by an ongoing bacterial infection when, in fact, the cause is not currently known.”
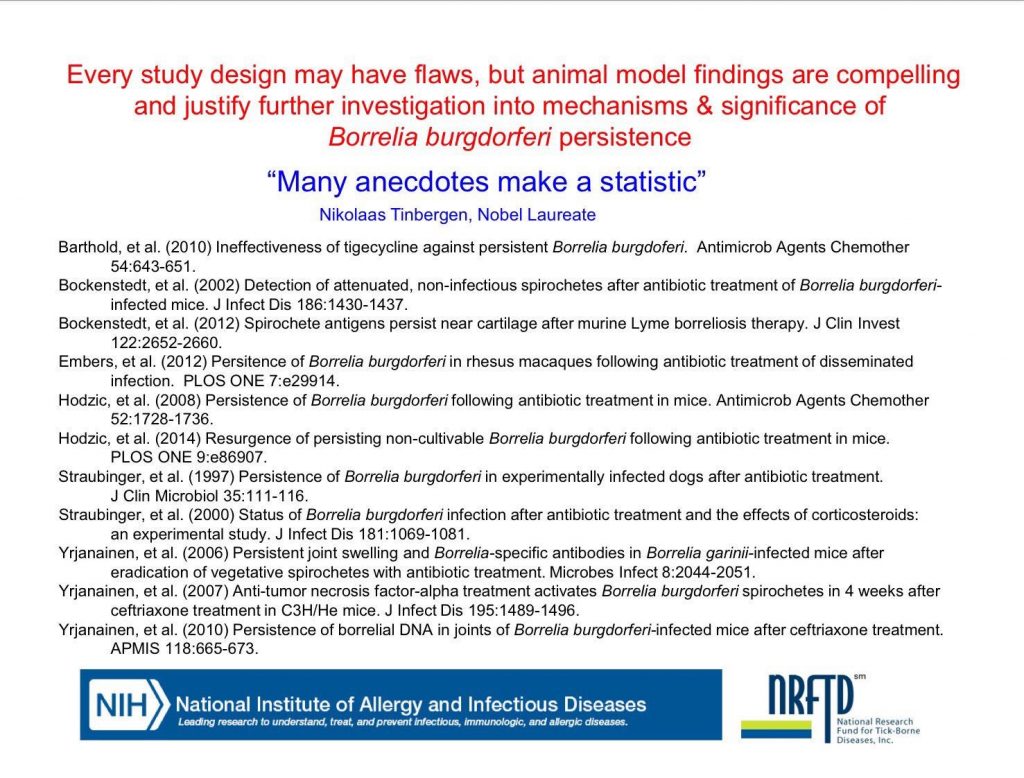
- I don’t even know where to begin here. See my prior writings on persisting bacterial infection here, here and here.
- Even better, how about this screen shot from an HHS Special Webinar on Lyme Disease Persistence showing Borrelia persistence in multiple animal models:
Treatment of Prolonged Symptoms
The CDC states: “Careful studies conducted over the last two decades in the United States and Europe have generally found that extended treatment with antibiotics is no better than placebo for curing prolonged symptoms.”
- In MyLymeData, longer antibiotic treatment durations were associated with better treatment response — with most well patients reporting treatment durations of four or more months.
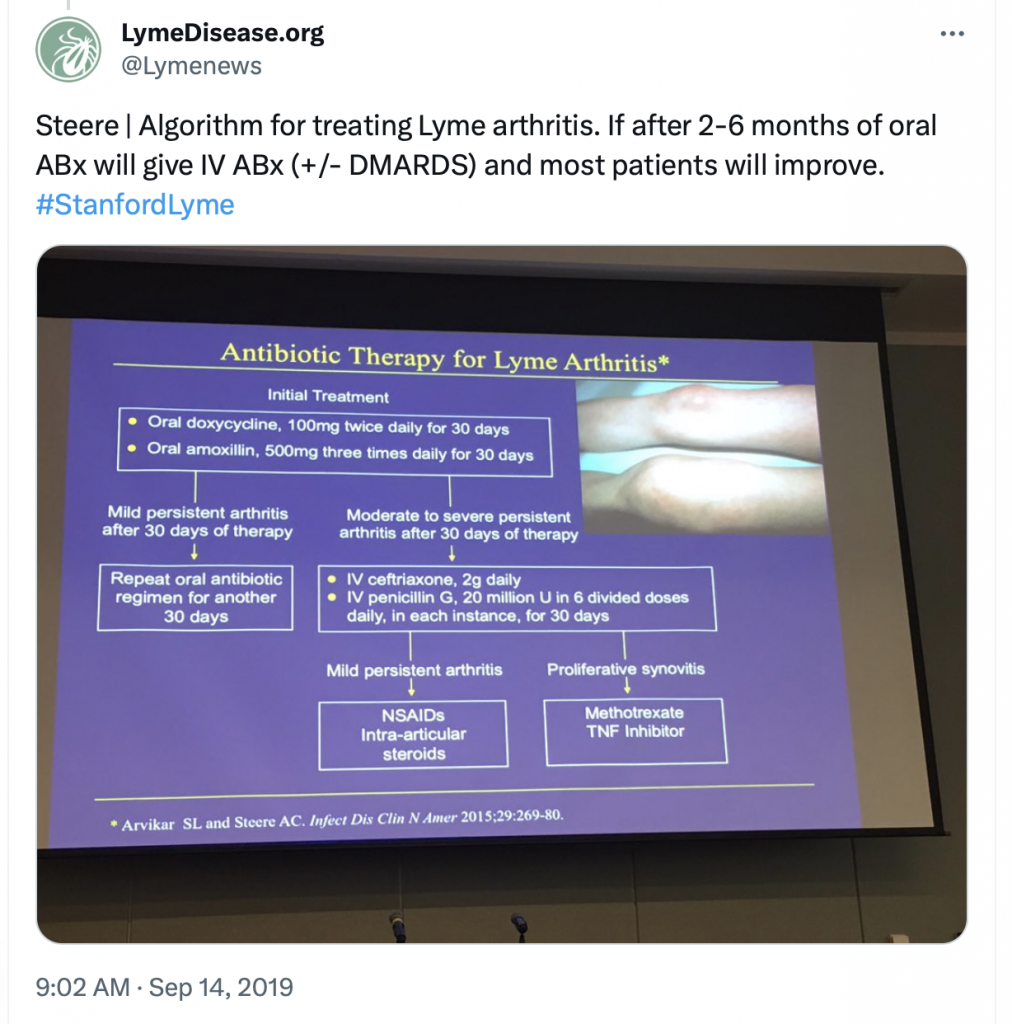
- Even Dr. Allen Steere (who first identified the illness in children near Lyme, Connecticut) administers longer treatment durations for patients with persisting symptoms. In 2019, I attended Stanford’s first Continuing Medical Education (CME) conference focused on tick-borne diseases. At that event, Dr. Steere presented his treatment protocol for Lyme arthritis. Basically, Steere said that if a patient has persisting symptoms after two or more months of oral antibiotics, he gives IV antibiotics with or without DMARDS (disease-modifying antirheumatic drugs) and most patients will improve. Here is a link to my live tweets of Steere’s lecture that day.
A Word of Caution
The CDC states: “It is especially unlikely that Lyme disease is the cause of prolonged or recurring symptoms if you tested negative for Lyme disease using a recommended test…”
- Umm, talk about confusing. The CDC’s “recommended test” for Lyme disease detects antibodies that may take 4-6 weeks for the patient’s immune system to produce. It is a strict test, with very few false positives, that was designed for surveillance. Because of this, the CDC states (on a different page) “Lyme disease is diagnosed based on: signs and symptoms, and a history of possible exposure to infected blacklegged ticks.” What this means is that early treatment for Lyme disease is based upon a clinical diagnosis and is not dependent on a test that is prone to false negatives. So why are they saying on this page that a negative test is absolute?
- At best, the standard test for Lyme disease misses 50% of the cases. And when antibiotics are given early, some patients will never develop the antibodies detected by the standard test. Even the IDSA’s case definition acknowledges that B. burgdorferi antibody levels are not sensitive or specific enough to distinguish when the infection has been cleared by antibiotics.
- And while it’s true that prolonged symptoms could be associated with a tick-borne co-infection, it seems logical to assume that if the patient tested positive for Lyme disease, their prolonged symptoms are related to Lyme until proven otherwise.
Don’t Give Up Hope
I’m not giving up hope, and neither should you. As Dr. John Aucott of Johns Hopkins acknowledges “The true extent of this insidious epidemic is still unknown, but it is clear, based on my experience and work, that it’s no longer accurate to simply argue that chronic Lyme disease doesn’t exist.“
This week the HHS published its national Vector-Borne Disease Strategy. It identifies and describes federal priorities to detect, prevent, respond to, and control diseases and conditions caused by vectors—disease-carrying insects and arachnids, such as ticks, mosquitoes and lice.
In 2019, Congress passed the Kay Hagan Tick Act. As stipulated by that law, HHS and CDC consulted the Tick-Borne Disease Working Group (TBDWG) while developing the interagency strategy. During its six years of operation, the TBDWG provided three reports to Congress–all are worth reading.
This is progress folks, but Lyme disease research needs your help to be funded and continue. If you haven’t already, please register for the 2024 virtual Lyme Fly-in. (Note: deadline to register to participate is Feb. 10.) We have more work to do.
LymeSci is written by Lonnie Marcum, a physical therapist and mother of a daughter with Lyme. She served two terms on a subcommittee of the federal Tick-Borne Disease Working Group. Follow her on Twitter: @LonnieRhea Email her at: lmarcum@lymedisease.org.
References
Aucott JN, Rebman AW, Crowder LA, Kortte KB. (2013) Post-treatment Lyme disease syndrome symptomatology and the impact on life functioning: is there something here? Qual Life Res. doi: 10.1007/s11136-012-0126-6. PMID: 22294245; PMCID: PMC3548099.
Aucott JN, Yang, T, Yoon I, Powell D, Geller SA, Rebman AW (2022) Risk of post-treatment Lyme disease in patients with ideally-treated early Lyme disease: A prospective cohort study, Int’l J. of Infectious Diseases (2022), doi: https://doi.org/10.1016/j.ijid.2022.01.033
Johnson L, Stricker RB. (2004) Treatment of Lyme disease: a medicolegal assessment. Expert Rev Anti Infect Ther. doi: 10.1586/14787210.2.4.533. PMID: 15482219.
Johnson, Lorraine (2019): 2019 Chart Book — MyLymeData Registry. (Phase 1 April 27, 2017. Sample 3,903). https://www.lymedisease.org/mylymedata-lyme-disease-research-report/




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page