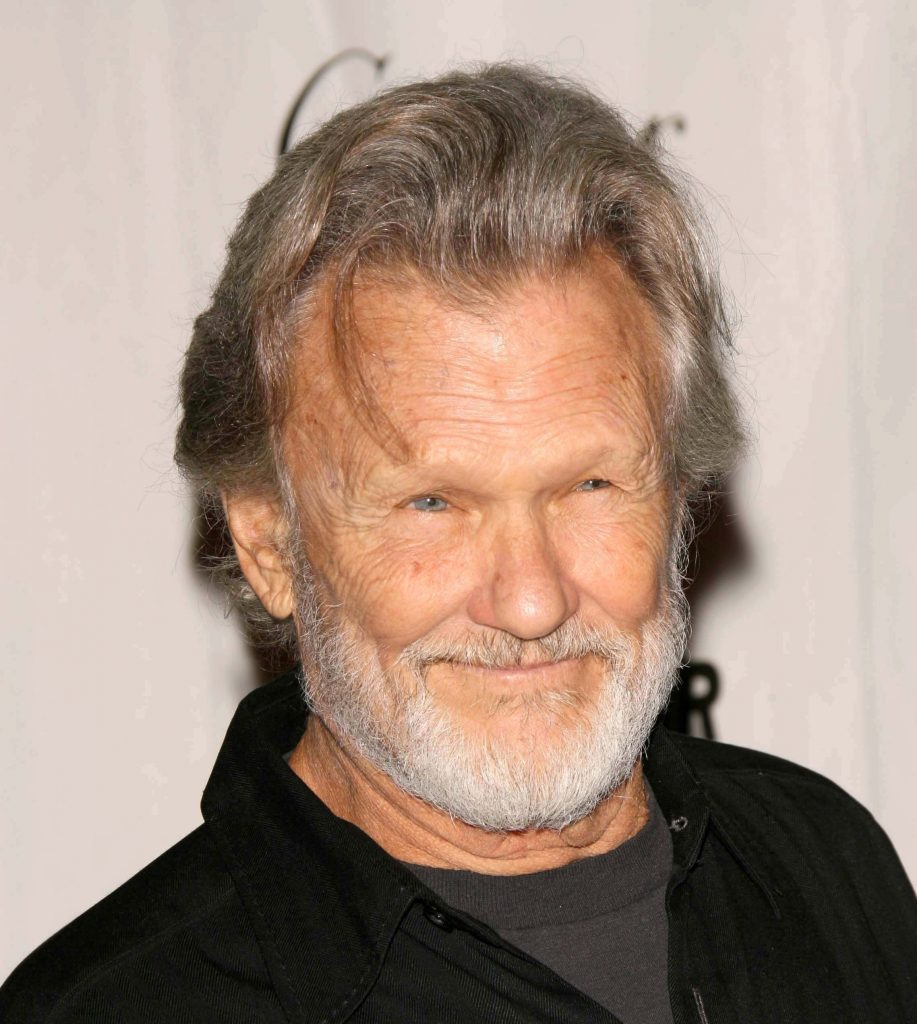
MEDICAL DETECTIVE #5: Kris Kristofferson had chronic Lyme–not Alzheimer’s. How can you tell the difference?
This article was originally posted on Dr. Richard Horowitz’s Medical Detective Substack. You can find more helpful content by subscribing there.
I remember seeing the late Kris Kristofferson (KK) for the first time when he starred with Barbara Streisand in “A Star Is Born.” He was already an accomplished singer/songwriter/actor and got a Golden Globe award for that performance.
Whenever someone of great musical talent is recognized for other genres (like Lady Gaga, now starring in “Joker: Folie à Deux,” and who starred in a remake of “A Star is Born” with Bradley Cooper in 2018) it makes me appreciate such talent even more.
Especially to hear Gaga go from “Just Dance” to “Shallow” to Tony Bennett duos. That takes chutzpah (Yiddish for “balls”) and an awful lot of talent. It also makes me hope that someday I might break out of my genre and become known for my stand-up-medical comedy, not just as someone helping to find treatment solutions for world-wide epidemics!
I have so much material after 40 years in medicine that there has to be a way to share it so we can poke fun of our dysfunctional medical system. And I like to make patients laugh.
Why was Kristofferson’s diagnosis missed?
First of all, if a doctor only takes 15-20 minutes with a patient (in an HMO model), that is only about enough time to dive down deeply with 1-2 symptoms. Not the 38+ symptoms that show up routinely in chronic Lyme patients. I imagine KK’s medical team took more time because of who he was, but inherent bias in diagnoses is not uncommon.
Doctors believed KK had Alzheimer’s disease (AD) due to multiple head injuries when he was young (playing rugby, football, and boxing), which can be associated with neurological inflammation later in life (neuro-inflammation) and cause a dementia-like illness.
In fact, in people with Major Neurocognitive Disorders (MND), there are 13 possible causes. They include Alzheimer’s disease, vascular disease, frontotemporal lobar degeneration, Lewy body disease, Parkinson disease, HIV infection, Huntington disease, prion disease, substance and/or medication use, traumatic brain injury, another medical condition, multiple etiologies, and unspecified. This comes directly out of the peer-reviewed medical literature.
It’s the “another medical condition” and “multiple etiologies” that specifically interest me. A patient may have more than one etiology contributing to MND, but a medical history of multiple head traumas earlier in life often influences the diagnostician.
Don’t assume
The Medical Detective has to be careful not to assume anything and take the time to do a comprehensive history and physical. One way to ensure a doctor is getting the full picture is to have the patient take my validated Lyme symptom questionnaire (HMQ), score it, and see the pre-test probability of infection. The HMQ can be downloaded from our website, Can Get Better.
In KK’s case, the risk was high. He had previously been diagnosed with fibromyalgia, a known mimic to Lyme disease, causing a chronic fatiguing, musculoskeletal, neuropsychiatric illness. His wife, Lisa Meyers, believes he contracted Lyme disease while filming the movie “Disappearances” in Vermont.
That state is a known hot spot for ticks, and he got ill after crawling around for days in a forest. Hmmm, got sick after crawling around in a forest. I wonder what that could be. Medical Detective’s first clue: getting the above symptoms after being in the woods in known highly tick-endemic areas and scoring high on the HMQ with migratory pain.
This would have indicated a very high probability of exposure to Borrelia burgdorferi, the agent of Lyme disease. Then getting a Lyme Immunoblot from IgeneX labs, and playing Lyme Bingo–looking for one or multiple Borrelia-specific bands (23, 31, 34, 39, 83/93). Any one band in the right clinical setting helps to establish the clinical diagnosis.
Do you suffer from memory loss and concentration problems?
You will find on the list below the most common variables that have been associated with memory loss and Alzheimer’s dementia. You can see from this list that AD has been associated with multifactorial etiologies:
- Infections (spirochetes including Lyme disease [Borrelia burgdorferi], herpes viruses [HSV1, 2, HHV 7, HHV 8], chlamydia pneumonia, Porphymonas gingivalis, H. Pylori, Bartonella, Propionibacterium, COVID)
- Environmental toxins (pesticides, heavy metals)
- Mitochondrial dysfunction
- Microbiome abnormalities with or without leaky gut and mast cell activation
- Hormonal deficiencies (sex hormones, thyroid, insulin resistance, hypoglycemia)
- Sleep disorders (Delayed Sleep Phase Syndrome, i.e., DSPS, Obstructive Sleep Apnea)
- Medication side effects (PPIs, statins, psychiatric meds, anti-cholinergic drugs)
- Vitamin and Mineral Deficiencies (B vitamins, Vitamin D, et. al)
- Genetics (like Apo E, a known genetic risk factor)
- Alcohol disorder
- Blood Pressure (low blood pressure, POTS as well as hypertension with high blood pressure)
- Autoimmunity (PANS/PANDAS, autoimmune encephalopathy)
- Other factors (insulin resistance, depression, pain syndromes, deconditioning)
Now take a look at the same etiologies found on the 16-point MSIDS map that have been associated with chronic inflammation and memory/concentration problems:
16 Point MSIDS Map: Sources of Inflammation and Downstream Effects Associated with Chronic Cognitive Dysfunction
Primary Sources
- 1) Chronic infections
- A. Bacteria: spirochetes like Lyme disease, Bartonella spp., porphymonas gingivalis, H. pylori, Propionibacterium
- B. Viruses: herpes viruses, COVID
- C. Parasites: Babesia, Malaria, Toxoplasma, Echinococcosis (hydatidosis) Schistosomiasis, Paragonimiasis, Toxocariasis, Onchocerciasis
- D. Fungi: Aspergillus, Cryptococcus, Candida, Mucorales, dematiaceous molds, and dimorphic endemic fungi
- 2) G.I.: Dysbiosis of intestinal bacteria, reduction of Clostidiaceae (Clostridium sensu stricto 1) and increases in Enterobactericeae and Bacteroides
- 3) G.I.: Leaky gut with food allergies and sensitivities/mast cell activation
- 4) Sleep disorders: lack of proper sleep (sleep apnea, infections with DSPS [Delayed Sleep Phase Syndrome], shift worker syndrome, menopause, BPH)
- 5) Environmental toxins: heavy metals, mold, pesticides, VOS’s, etc.
- 6) Nutritional deficiencies: zinc, copper, magnesium; B1, B6, B12, folate, vitamin D
- 7) Nutritional overload (copper, Wilson’s disease; iron, hemochromatosis)
Downstream Effects
- 8) Endocrine disorders: low testosterone, low estrogen, menopause, low adrenal function, hypothyroidism, low blood glucose (hypoglycemia)
- 9, 10) Neurological, Psychological dysfunction: strokes, PTSD with trauma, amyloid/tau buildup, tumors
- 11) POTS/dysautonomia with low blood pressure
- 12) Mitochondrial dysfunction: genetic or acquired, affects all organ systems including memory/concentration
- 13) Pain syndromes: pain decreases cognitive processing; can affect long-term memory, selective attention, processing speed, and executive functioning
- 14) Liver dysfunction: cirrhosis or fatty liver (NASH: Nonalcoholic steatohepatitis) with elevated ammonia, severe hepatitis B or C infection, alcohol abuse, autoimmune hepatitis, bile duct disorders, some medicines affecting the liver
- 15) Autoimmune phenomenon (PANS/PANDAS, AI encephalopathy)
- 16) Medication side effects: benzodiazepines, opioids, antipsychotics, anticholinergics, antiepileptics.
The two lists overlap. Alzheimer’s disease is a multi-factorial illness
You will notice that the two lists completely overlap! The majority of the variables found on the 16-point MSIDS map associated with chronic inflammation can cause memory/concentration problems with poor cognition.
Although association does not prove causality, there is now accumulating scientific evidence linking Alzheimer’s disease to spirochetal infections like Lyme disease (as well as other infections, like viruses).
In fact, an article published in the 2022 peer-reviewed literature indicates that Borrelia burgdorferi (the bacteria causing Lyme disease) co-localizes with amyloid markers in AD brain tissues. Lyme disease has previously been published in the Journal of Alzheimer’s Disease as a potential factor causing dementia, and has been shown to be associated with chronic inflammation in the brain, causing amyloid production.
So, any MND has 13 potential subtypes and 16 potential overlapping causes. You can have Lyme disease and head trauma causing inflammation. Pesticides, heavy metals, mold, and/or microplastics in your brain can all cause inflammation, along with Lyme disease and head trauma.
The key is to identify all potential overlapping causes of inflammation and downstream effects, and address them all to maximize the patient’s health and chance of recovery. When the typical AD drugs given to KK were ineffective for dementia and depression–and he had physical symptoms, not just memory problems–that was an indication something else was going on.
Moving from a one-cause/one disease model
A basic medical dysfunction woven into our healthcare system may or may not have also played a role in the initial misdiagnosis of AD in KK’s case. First of all, most chronic medical problems are still approached from the 1800s model from Pasteur and Koch–that there is one cause for one disease.
That doesn’t work for chronic disease medicine, where many chronic illnesses are either due to Lyme-MSIDS (Borreliosis with multiple inflammatory triggers and downstream effects) or Non-Lyme MSIDS (other infections and/or inflammatory triggers with downstream effects).
The other problem is that doctors often like to name a disease and throw a drug at it. You may not know that pharmaceutical companies provide the majority of funding of medical schools…which might have something to do with it. So, when you approach AD with the notion that you should pull amyloid plaques out of the brain–the focus of some present treatments for AD–without getting to all of the underlying factors causing the memory/concentration problems, you risk the chance of missing treatable causes.
The message you need to know
Most chronic diseases have a multifactorial etiology. When I recently published my long-term follow-up of three patients with chronic Lyme disease in the journal Microorganisms, who were all-in long-term remission after dapsone combination therapy, I also showed that long COVID has been associated with all 16 points on the MSIDS map as well. (Horowitz, R.I.; Fallon, J.; Freeman, P.R. Combining Double-Dose and High-Dose Pulsed Dapsone Combination Therapy for Chronic Lyme Disease/Post-Treatment Lyme Disease Syndrome and Co-Infections, Including Bartonella: A Report of 3 Cases and a Literature Review. Microorganisms 2024, 12, 909. https://doi.org/10.3390/microorganisms12050909)
It’s the same situation for AD and MNDs. We need to shift from a one-cause, one disease model in chronic disease medicine, and consider using the 16-point MSIDS model as a starting point to make sure we don’t miss treatable causes.
Especially because BMJ Global Health recently published that roughly 1 out of 7 people on the planet have now been exposed to Lyme disease (14.5%), and the CDC had to revise their estimates of exposure earlier this year, from 476,000 people a year in the US getting Lyme, to the figures being 1.7 x higher, with Medicare rates being even 7 x higher!
That gets us to roughly 3 million Americans per year who are exposed to a tick-borne infection that causes severe memory/concentration problems. Maybe that should be in the forefront now whenever anyone comes into a doctor’s office with memory/concentration problems.
The growing epidemic
Lyme is in epidemic proportion. Based on what I am seeing in my medical office, so is Bartonella, Babesia, mold toxicity, heavy metal toxins, POTS, low hormones, sleep disorders, metabolic syndrome with insulin resistance, depression, vitamin and mineral deficiencies, mitochondrial dysfunction as well as leaky gut, mast cell activation and microbiome imbalances.
All of these MSIDS factors can cause cognitive issues.
It’s high time for a paradigm shift in how we approach chronic illness. Especially in the middle of an expanding Alzheimer’s epidemic, where over 46 million people in the US have been diagnosed with pre-clinical dementia.
We can do better. How many of these individuals have been exposed to Lyme and multiple factors on the MSIDS map—and are misdiagnosed like KK was?
If you suffer from cognitive issues, don’t just accept a diagnosis of AD like KK did. It may turn out that you too had a treatable illness, and didn’t have to necessarily suffer.
This article was originally published on Substack by Dr. Richard Horowitz.
Dr. Horowitz has treated 13,000 Lyme and tick-borne disease patients over the last 40 years and is the best-selling author of How Can I Get Better? and Why Can’t I Get Better? You can subscribe to read more of his work on Substack or join his Lyme-based newsletter for regular insights, tips, and advice.
[Editor’s note: Kris Kristofferson passed away on September 28. 2024, at the age of 88. See also: Kris Kristofferson’s shocking tale of Lyme-induced Alzheimer’s, by Dana Parish.]




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page