Why some people with Lyme disease don’t test positive for it
By Nancy Dougherty
The immune response in Lyme disease has been described as dysregulated or maladjusted.
This is supported in part by the fact that many individuals who clearly have Lyme disease do not make a detectable immune (antibody) response to Borrelia burgdorferi (Bb), the tick-borne pathogen that drives the disease.
Research at the Johns Hopkins University School of Medicine may provide insights into why this occurs.
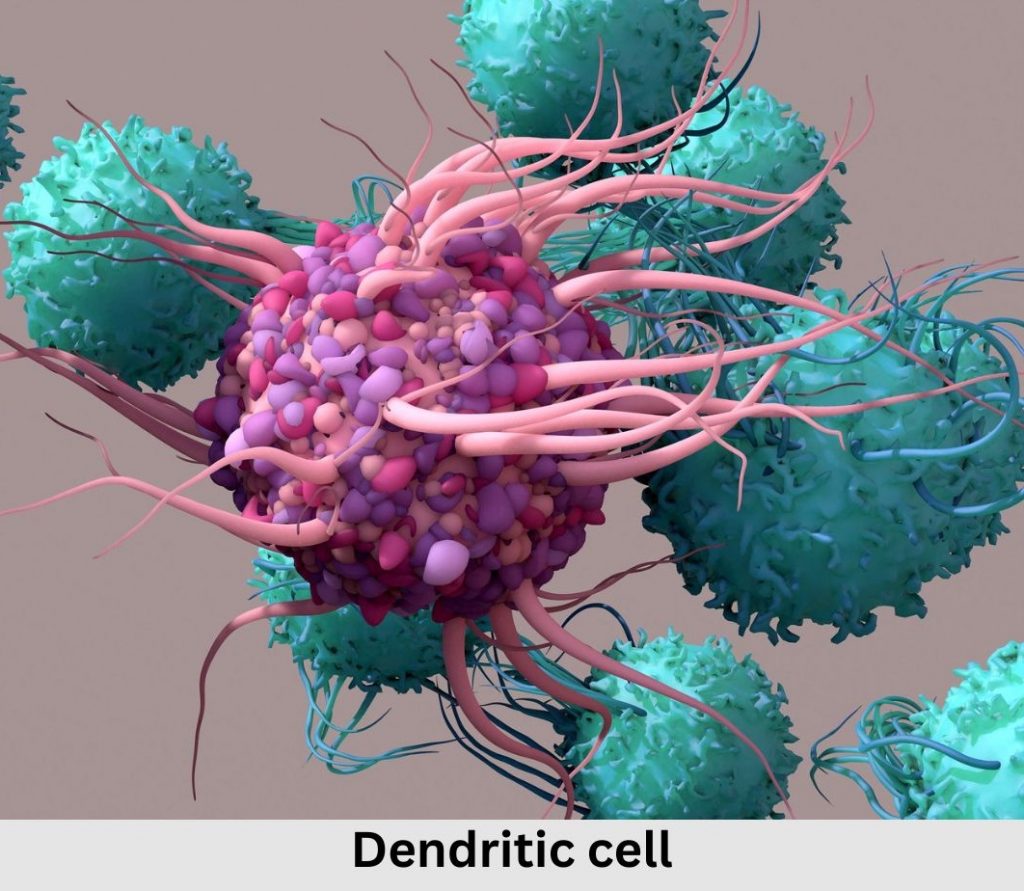
Dendritic cells (DCs) are a broad class of immune cells that reside at strategic sentinel sites in the body, including the skin and GI tract.
Dendritic cells stand watch for pathogens
DCs constantly monitor their environment by gobbling up the fluid that surrounds them to sense when pathogens arrive on the scene. When they detect a pathogen, DCs stop capturing material and move to the closest lymph node.
There, DCs interact with T lymphocytes (T cells) to activate and drive pathogen-specific T cells to help initiate a strong immune response to clear the pathogen and resolve the infection.
When everything is working right, activated dendritic cells provide three signals to T cells (signals 1, 2 & 3) that synergize to generate a strong T cell activation.
In a 2023 Johns Hopkins study, using proteomics and genomics-based approaches, researchers found that DCs exposed to Borrelia burgdorferi were fully capable of generating signal 1 but signals 2 & 3 were abnormal. In fact, the features discovered overlapped with what is found in a tumor microenvironment, a site where immune responses are known to be suppressed and dysregulated.
A lead author of the publication, Mark Soloski, PhD, Professor Emeritus, Johns Hopkins University School of Medicine, divulges, “It has been known for some time that Borrelia burgdorferi is highly capable of evading the immune response, and this disruption of dendritic cell activation signaling is likely another clever way that Borrelia mutes the immune response.”
He adds, “Further study is needed to better understand the precise nature of the dendritic cell driven T cell responses in patients with Lyme disease.”
There are immediate implications, however.
Clearly, antibody-based diagnostic tests (the current standard) are going to miss those who are not making a normal antibody response due to Borrelia burgdorferi’s immune response disrupting behavior.
The need for direct testing
The need for effective direct diagnostic tests that identify Bb DNA or proteins directly has never been more obvious. Misdiagnosis and delayed diagnosis are indeed a common Lyme disease occurrence. Resulting treatment delays lead to worse prognoses, including potentially disabling chronic illness.
Fifty years after the discovery of Bb as the causative agent of Lyme disease, there are still no FDA-approved direct diagnostic tests for Lyme disease or treatments for persistent Lyme disease. These need to be developed, validated, and become broadly available.
Given that dendritic cells play such a key early role in immune response initiation, the novel features identified in Borrelia burgdorferi exposed cells may suggest new therapeutic targets that could help generate stronger, more robust immune responses in Lyme disease that could result in enhanced bacterial clearance and disease resolution. Immune modulators are effective therapeutic targets in cancer and could be promising therapeutic approaches for Lyme disease as well.
Nancy Dougherty is an education and communications consultant for the Johns Hopkins Lyme Disease Research Center.




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page