LYME SCI: Tick-borne Powassan virus can be deadly
After the 2017 death of two men in Cape Cod, many people are learning for the first time that ticks can carry viruses too, not just bacteria like Lyme disease. And that such tick-borne viruses can pose a significant threat to public health.
Powassan virus (POWV) is considered an “emerging infectious disease,” though it is not new. In fact, the first case was discovered in 1958 in the small town of Powassan, located in Ontario, Canada.
A Massachusetts case had a better outcome. Tucker Lane contracted Powassan in 2014 and considers himself lucky to be alive.
Lane “woke up sweating, cold, shaking… felt like I was going to puke,” he told CBS Boston. A few days later, he fell into a week-long coma. “They kind of told my parents there’s nothing more we can really do.” Eventually, however, he came out of it.
Three years later, Lane says his health is fine and he reports no lingering symptoms or damage to his brain. “I knew I got lucky in a very unlucky situation,” Lane said.
Symptoms
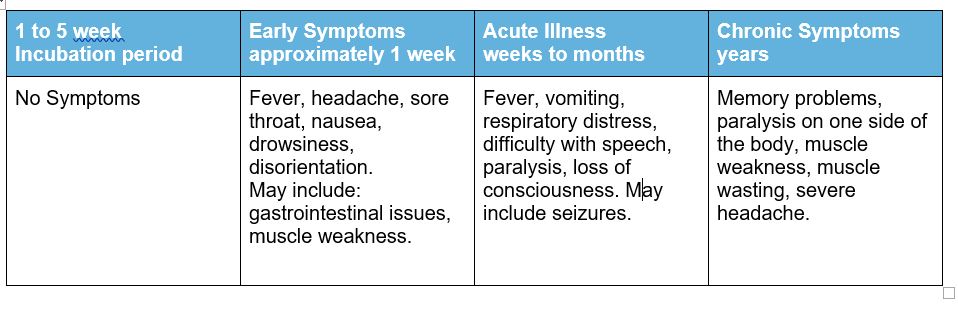
For those who become ill, the symptoms of POWV develop anywhere from 8-34 days after the tick bite. The initial symptoms are flu-like with a fever.
If the infection spreads to the brain, severe neurological symptoms can develop, including strong headache, mental confusion, paralysis, seizures and unconsciousness. About 60% of patients who survive the infection are left with permanent neurological dysfunction including partial paralysis, headaches, memory impairment and paralysis of the eye muscles. Nearly 10% of Powassan cases are fatal.
No cure
Currently, there is no cure for POWV. Many of the patients who develop symptoms need to be hospitalized. The treatment consists of IV fluids, anti-inflammatories and in some cases, breathing and life support.
Powassan is a Flavivirus which is related to Zika, Dengue, West Nile, and tick-borne encephalitis virus (TBEV). They are named Flava (which means yellow in Latin) after the Yellow Fever virus that causes yellowing (jaundice) of the skin. Flaviviridae are a family of viruses that can cause brain swelling (encephalitis).
Emerging infectious diseases
Powassan and many other tick-borne diseases are considered emerging because the number of cases has increased significantly over recent years. There is some debate over whether increased geographic spread or better detection techniques has led to the increased number of reported cases. I suspect both factors play a role. (see Ehrlichia another emerging infectious disease)
One way to determine whether POWV is spreading is through tick studies. There seems to be great variation from year to year but studies show anywhere from 1% to 10% of ticks in endemic states test positive for POWV compared to 20%-50% for Lyme.
Two types of Powassan in North America
There are two types of Powassan in North America. Lineage 1 POWV is associated with both woodchucks and Ixodes cookei ticks; or squirrels and Ixodes marxi ticks. Lineage 2, sometimes called deer tick virus (DTV), is associated with the white-footed mouse and Ixodes scapularis ticks.
Because I. cookei and I. marxi do not climb up blades of grass in wait for a suitable host (a behavior known as questing), they are not thought to play a major role in the transmission of POWV.
The backlegged or “deer tick” (Ixodes scapularis) on the other hand, has developed multiple strategies for questing. Deer ticks are also aggressive biters, making them much more competent in transmitting diseases like POWV to humans.
Add Powassan to the tick toxic soup
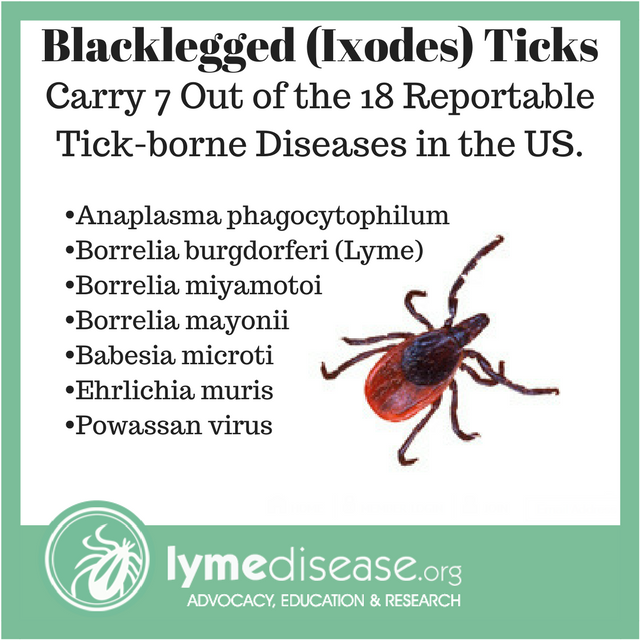
While many tick species are known to carry POWV, the blacklegged tick (I. scapularis) is the primary vector. Blacklegged ticks can carry many pathogens and can transmit more than one infection in a single bite. While we should be very concerned about POWV, the risk of contracting Lyme or Babesia is currently much greater. (See my previous post on co-infections)
No grace period
A tick becomes infected with POWV after feeding on a small mammal carrying the virus. When the infected tick bites a human, transmission can occur in as little as 15 minutes. Since ticks are so small and POWV transmission so rapid, very few patients with Powassan encephalitis will recall the tick bite.
If you get bitten by a tick while out hiking or playing, you could be infected with Powassan without even realizing anything has happened.
Hidden epidemic?
Most Powassan virus infections are thought to be asymptomatic. This assumption is based, in part, on reviewing the results of human blood tests. Two studies found that 0.7% of New Yorkers and 3% of Canadians from Ontario carry antibodies to POWV—meaning they were infected at some point.
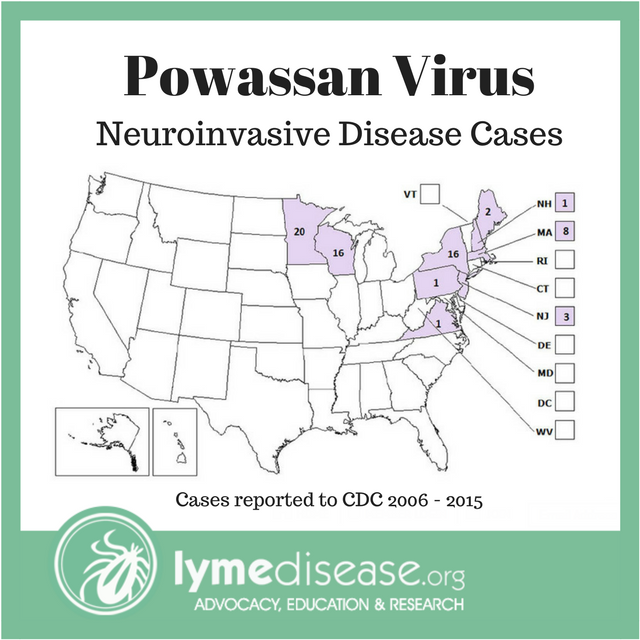
Rough math says 0.7% of New Yorkers would make 500,000 cases of POWV in that state alone, when in fact, only 16 cases were reported in New York from 2006 to 2015. This suggests that the majority of cases are asymptomatic, and that POWV is underrecognized as an infectious disease.
Unrecognized POWV may also contribute to the high number of Lyme disease patients who remain ill after treatment, because viruses do not respond to antibiotics. Some experts theorize that POWV and other viruses may also play a part in other chronic neurologic diseases, like lupus, multiple sclerosis, ALS, Parkinson’s, chronic fatigue syndrome or myalgic encephalomyelitis. But this is still under investigation.
Timeline of Illness
Geographic distribution
The underdiagnosis of POWV contributes to the lack of understanding of the geographic distribution. From 2006 to 2015, there were only 68 cases of POWV reported to the CDC with eight (12%) fatalities. (see map)
After the sudden death of a women in Maine in 2013, that state conducted its own tick study on the Powassan virus. The researchers tested a total of 1,729 I. scapularis ticks from 30 different locations statewide and the results were astonishing.
The rate of infection throughout Maine ranged from a low of 0% to a high of 16% (average 7% adult, 9% nymphs). “We were kind of surprised that we found as much as we did,” said Chuck Lubelczyk, the project director.
POWV has been established along the East Coast from Virginia to Nova Scotia, throughout New York, Pennsylvania, Michigan, Wisconsin and Minnesota, broadly throughout Canada, and in rare instances has been detected in Colorado and California.
There are other several other tick-borne viruses found in the US, including Heartland virus, Bourbon virus and Colorado tick fever, which will be addressed separately.
As with all tick-borne diseases, prevention is key. Click here for more information about protecting yourself, your family and your pets.
LymeSci is written by Lonnie Marcum, a Licensed Physical Therapist and mother of a daughter with Lyme. Follow her on Twitter: @LonnieRhea Email her at: lmarcum@lymedisease.org .
References
Centers for Disease Control (CDC) Powassan Virus
Powassan Virus: An Emerging Arbovirus of Public Health Concern in North America
Powassan virus disease cases and deaths reported to CDC by year and clinical presentation, 2006-2015
Four emerging arboviral diseases in North America: Jamestown Canyon, Powassan, chikungunya, and Zika virus diseases
Emerging Causes of Arbovirus Encephalitis in North America: Powassan, Chikungunya, and Zika Viruses
ThomasLA, KennedyRC, EcklundCM. Isolation of a virus closely related to Powassan virus from Dermacentor andersonii collected along north Cache la Poudre River, Colo. Proc Soc Exp Biol Med 1960; 104:355–359
JohnsonHN. Isolation of Powassan virus from a spotted skunk in California. J Wildl Dis 1987; 23:152–153
Powassan Encephalitis Virus in Deer Ticks (Ixodes scapularis) in Maine (2015-2016). Main Department of Agriculture, Conservation and Forestry.




















Thank you for this very educational, detailed Powassaj virus. I learned a lot from it. I hope you post this on Facebook for others to learn also. Thank you
I n Canada nothing is being done to test people for Lyme disease, and offer no treatment. if someone has it. witch is frightening!
bourbon virus death in Missouri
http://www.emissourian.com/local_news/county/bourbon-virus-linked-to-death-of-park-official–/article_057f0f0a-bddd-5f7a-aa0d-735187e4c379.html