A decade ago, LymeDisease.org introduced MyLymeData, now recognized as the largest patient-driven registry for Lyme disease in the United States.
What is a patient registry? It’s a system that collects information about patients with the same medical condition, in order to figure out the best ways to improve their care.
Why is this significant? Because before MyLymeData, there was little real-world information about the many ways that Lyme disease affects individuals, especially those who stay ill for months or years.
Unlike traditional research models, MyLymeData puts the power of information directly into the hands of patients, enabling them to share their experiences.
It seeks to answer pressing questions like: What are the most debilitating symptoms for Lyme disease patients? Are there treatments that provide effective relief? If so, which treatments have proven the most helpful? Does Lyme disease manifest differently in women compared to men? These are not just abstract scientific queries, they are life-altering concerns for thousands of people. More and more, the research world is paying attention.
Shining a light, pointing the way
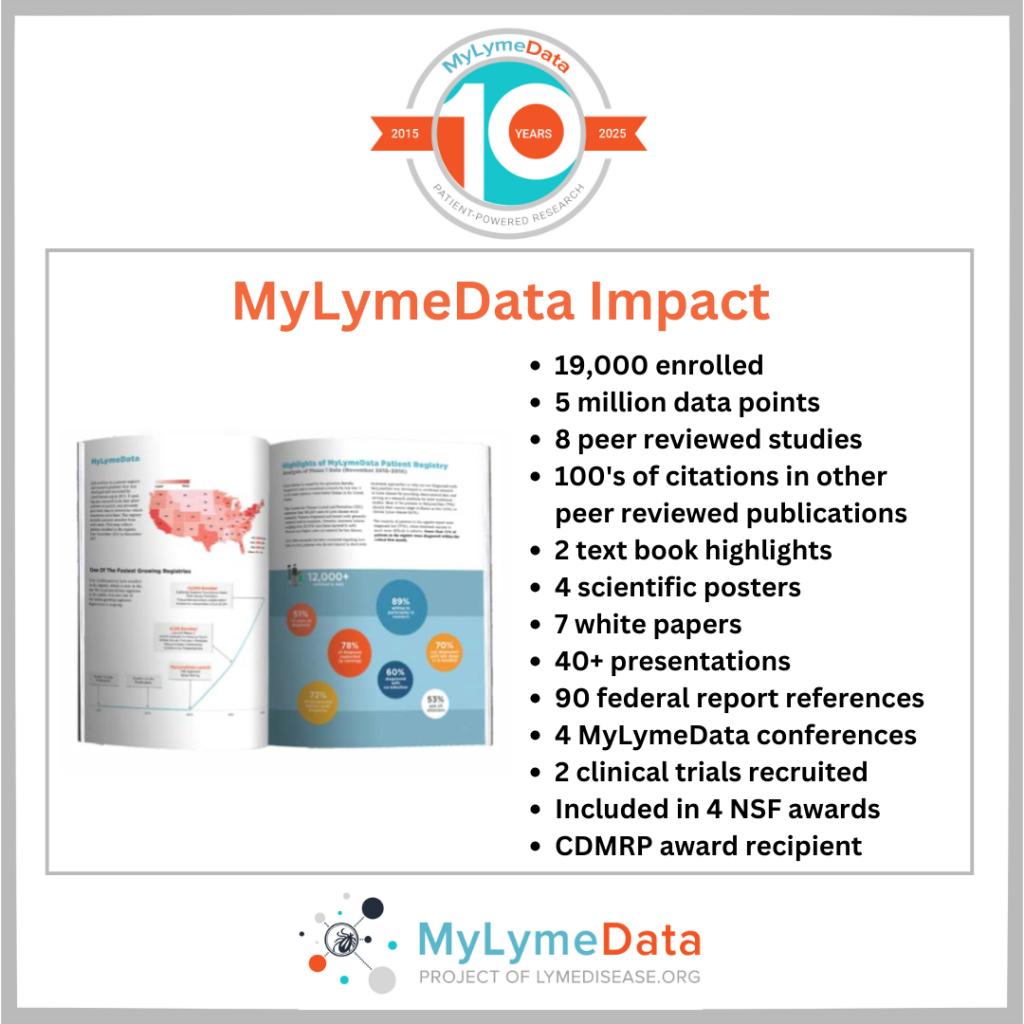
Since its debut in 2015, MyLymeData has enrolled over 19,000 participants, collecting millions of data points. This invaluable resource shines a light on such critical issues as diagnostic delays, co-infections, treatment outcomes, and the profound effects of tick-borne diseases on patients’ overall quality of life. Importantly, it can help point researchers into promising directions.
Here are two examples of recent peer-reviewed studies from MyLymeData:
Study shows 90% of persistent Lyme patients excluded from clinical trials
There are sex-based differences in Lyme disease. Why this matters.
As MyLymeData marks its 10-year anniversary, we celebrate its important contribution—not only in gathering critical data, but in elevating patient voices and putting them at the forefront of Lyme disease research. Far more than just a database, this registry gives hope to those suffering from tick-borne illnesses, offering the possibility of better treatments and, ultimately, a cure.
If you’re a U.S. resident diagnosed with Lyme disease, consider joining MyLymeData today to help us achieve the milestone of 20,000 participants. Together, we can make meaningful progress in the fight against Lyme disease.
TOUCHED BY LYME is written by Dorothy Kupcha Leland, President of LymeDisease.org. She is co-author of Finding Resilience: A Teen’s Journey Through Lyme Disease and of When Your Child Has Lyme Disease: A Parent’s Survival Guide. Contact her at dleland@lymedisease.org.
By Meg Muckenhoupt
Missouri State Representative Matthew Overcast, Esq. has introduced a bill to add alpha-gal syndrome (AGS) and Lyme disease to that state’s list of mandatory reportable conditions.
AGS is an allergy to red meat and meat-related products that is triggered by a tick bite.
HB 986 also requires the Missouri Department of Health and Senior Services to submit annual reports on the incidence of AGS and Lyme disease to the federal Centers for Disease Control and Prevention.
Overcast says that alpha-gal syndrome profoundly impacts many individuals and families in his district. However, he needs hard data to persuade his fellow legislators to help solve this problem.
Many states at the epicenter of the AGS explosion don’t even mention AGS in their information about tick-borne diseases. If they do mention AGS, they don’t give a figure for the number of cases. Thanks to research by the US military, though, we can estimate the number of AGS cases in several states. That number is frighteningly large.
By testing the blood of 3,000 recruits for the allergic antibody to alpha-gal, researchers were able to identify AGS hot spots. In the most impacted states–like Arkansas, Oklahoma, Missouri, and Kansas–more than 20% of recruits tested positive. In some areas of these states, almost half the recruits had the antibody.
In Missouri, almost 30% of recruits had the alpha-gal allergic antibody. Extrapolating from this data, an estimated 80,000 Missourians may have AGS.
Documenting the extent of AGS and Lyme disease and tracking their expansion is the first step in attracting the public health resources needed for provider education and other help for people with AGS and Lyme.
If you are a Missourian affected by AGS and/or Lyme disease, please contact your state representative now to help pass HB 986.
Meg Muckenhoupt works with Alpha-gal Information, an Alpha-gal Alliance project.
From the Tick Boot Camp podcast:
Join us as we interview Dr. Steven Harris, a leader in chronic Lyme disease treatment, live from the International Lyme and Associated Diseases Conference.
Dr. Harris has been treating complex chronic illnesses for over two decades, pioneering integrative and personalized approaches for Lyme disease, tick-borne infections, ME/CFS, mold/mycotoxin illness, and more.
He is president-elect of ILADS.
Key Takeaways:
- A Legacy in Lyme Disease: Dr. Harris’ deep roots in the Lyme community, with his father being an early pioneer in Lyme diagnostics.
- Evolution of Treatment: From antibiotic-centric approaches to a more comprehensive, individualized treatment model.
- Addressing Chronic Lyme’s Complexity: Insights into the multi-systemic nature of the illness and the role of regenerative medicine.
- “Order of Treatment” Approach: A sneak peek into Dr. Harris’ upcoming book, which outlines his strategic framework for treating chronic illness.
- PARM vs. Harris’ Approach: How his method compares with the Prehabilitation, Assist, Rehabilitation, Maintenance (PARM) model.
Listen to the Tick Boot Camp podcast here, or via all major podcast streaming services such as Apple Podcasts, Spotify, and YouTube Music.
By Fred Diamond
When people talk about chronic Lyme disease, the conversation often turns to co-infections, immune dysfunction, and the heartbreak of being misdiagnosed. But increasingly, another word keeps coming up: mold.
In this week’s episode of the Love, Hope, Lyme podcast, I sit down with Ariana Thacker, founder of MoldCo, and Dr. Scott McMahon, a leading physician in mold-related illness, to talk about what happens when mold becomes a hidden yet devastating part of someone’s health crisis — especially when it intersects with Lyme disease.
What unfolds is a raw and informative conversation about lives upended, science overlooked, and a powerful new digital health company working to bring clarity and hope.
A Personal Descent into Mystery Illness
Ariana Thacker never expected her life to be derailed by something as mundane as mold.
“I’ve always been very healthy,” she says. But after moving into a condo in Miami, that started to change. Clumps of hair began to fall out. Brain fog and fatigue made it impossible to keep up with her fast-paced life. “There was a point where I was just taking my calls from bed. I wasn’t even able to walk upstairs without getting winded.”
Doctors couldn’t explain what was happening. A friend suggested mold might be the culprit, and when an independent inspector tested her home — not the one hired by her landlord — the results were staggering: dangerously high levels of toxic mold in the HVAC system and likely behind the walls.
That was her breaking point — and her breakthrough.
She began a journey of self-education, trial-and-error treatments, and eventually co-founding MoldCo, a digital health platform rooted in evidence-based protocols and real patient experience.
The Mold-Lyme Overlap
Dr. Scott McMahon is no stranger to mold illness. A pediatrician since 1992, he became immersed in the field after treating a cohort of students and a teacher from a high school where everyone seemed to be getting sick in similar, unexplained ways. With guidance from Dr. Ritchie Shoemaker — the pioneer of mold illness research — he ran advanced labs and saw shocking patterns: widespread immune dysfunction.
“Those who took the treatment and took it seriously, they all got better,” he says. “Those who didn’t, didn’t get better.”
Dr. McMahon says mold illness is called Chronic Inflammatory Response Syndrome (CIRS), and it’s far more than just a cough or a runny nose from a musty room. “It’s a multi-system illness that, if not treated, becomes progressive and can eventually become debilitating,” McMahon explains.
Cognitive problems, exhaustion, neuropathic pain, fibromyalgia-like symptoms, chronic headaches, digestive issues, disorientation, anxiety, and severe mood changes — these are just some of the hallmarks. The catch? Most of these symptoms mirror those of chronic Lyme disease.
“There’s a tremendous amount of overlap,” McMahon says. “So much so that if you don’t know what you’re looking for, it’s almost impossible to tell the difference.”
MoldCo: A Digital Lifeline
MoldCo isn’t just another telehealth startup. It’s a platform designed by mold survivors and mold-literate doctors to finally offer a clear, evidence-based path forward.
Now live in Texas and Florida, MoldCo offers what Ariana calls a “closed beta” — their early bird program. Patients meet with certified providers trained in mold illness, undergo advanced mold-specific labs, and receive prescriptions aligned with Shoemaker’s protocol. The entire experience is digital, affordable, and focused on one goal: giving people their lives back.
The MoldCo website offers a robust FAQ section, free checklists to assess your home for mold, and suggestions for at-home testing like ERMI or HERTSMI-2. They even provide access to air purifiers that use bipolar ionization, as a temporary solution while patients work to find clean housing.
“It’s not just about treatment,” Ariana says. “It’s about helping people get their environment under control too.”
Most importantly, MoldCo recognizes what Ariana herself went through — the medical gaslighting, the dismissal of symptoms, and the psychological toll. “Even after I told providers mold was the cause, they just weren’t equipped. They’d say, ‘That doesn’t cause health problems,’ or worse — ‘It’s all in your head.’”
Why Mold is So Hard to Diagnose
Despite its prevalence, mold illness remains largely ignored by mainstream medicine. Part of the problem, McMahon explained, is that most physicians aren’t trained to recognize it — or they lack the time.
“With today’s healthcare system, you get 15 minutes with your doctor,” he says. “If you walk in with 25 symptoms, they might only address two or three. You’re written off as mental, or they refer you to a psychiatrist.”
It’s a cycle Lyme patients know all too well. “Unless you’re looking for it, you won’t find it,” McMahon adds.
Even when patients do suspect mold, they’re often left on their own to find a reputable home inspector, order the right environmental tests, and piece together the right treatment plan. Many end up spending tens — even hundreds — of thousands of dollars, often without getting better. When someone is exposed to a moldy environment, they inhale spores and tiny fragments that trigger the body’s innate immune system — the first line of defense.
“Most people make antibodies and get over it,” McMahon says. “But mold-sensitive individuals don’t. Their immune system keeps reacting, over and over.”
This chronic immune activation spills into the rest of the body, disrupting everything from hormone levels to cognitive function, mood regulation, and energy metabolism. And much like Lyme, the illness doesn’t stop once the trigger is gone — it lingers until the immune system is reset through targeted treatment.
“I Didn’t Think I’d Ever Contribute Again”
One of the most powerful moments of the episode came when Ariana described just how devastating mold was for her — physically, mentally, and emotionally.
“I started mapping out a version of my life where I couldn’t contribute anymore,” she says. “I thought, ‘What if I’m just at this state forever?’” She slurred her words, couldn’t process spoken language, reread emails five times just to understand them, and withdrew from the world.
“I became a hermit.”
Meanwhile, she was bouncing from hotel to Airbnb, trying to find a “safe” environment — even as landlords denied responsibility and doctors told her she was fine.
“You’re failed at every level,” she says bluntly. “From the healthcare system to the legal system to housing protections. You feel like there’s no way out.”
So why does mold come up so often in Lyme conversations? Because the root dysfunction — immune system overactivation — is the same.
McMahon explained it like this: “The way different viruses can all cause the common cold, mold and Lyme can both trigger the same immune system pathway. The result is chronic inflammation that looks almost identical in both illnesses.”
Lyme and mold often come together
In fact, he believes many Lyme patients may actually have a mold component — and vice versa. That’s why it’s critical to look for both.
Despite the gravity of the topic, both Ariana and Dr. McMahon end our conversation on a hopeful note.
“There are resources,” McMahon emphasizes. “This is treatable. The earlier you get help, the better.”
Mold illness may be invisible, but it’s real. And for many Lyme survivors, it might be the missing piece of the puzzle.
As Ariana put it, “It just felt like a deterioration of everything. But once I understood what I was dealing with, I could finally start getting better.”
Click here to listen to all episodes of the Love, Hope, Lyme Podcast or on YouTube.
Fred Diamond is based in Fairfax, Virginia and can be contacted via Facebook. His popular book, “Love, Hope, Lyme: What Family Members, Partners, and Friends Who Love a Chronic Lyme Survivor Need to Know” is available on Amazon. The e-version of the book is always free to Lyme survivors. PM Fred on Facebook or LinkedIn for your copy.
By Shirley Mueller, MD
Well-known author Amy Tan had always been a keen observer of life’s subtle clues—after all, unraveling complex family sagas and hidden truths was her literary specialty. Nevertheless, nothing prepared her for the baffling mystery unfolding in her body.
It began quietly one warm July evening in 1999. Attending an outdoor wedding in Dutchess County, New York, Amy barely noticed the small bite on her shin, marked by a tiny black dot in the center of a bright red circle. Spider bite, she thought dismissively, brushing off the curious mark.
The next day, flu-like symptoms crept in—aches, fever, exhaustion. But just as quickly as they arrived, they disappeared, seemingly insignificant. She carried on, attributing lingering aches, stiff neck, and headaches to stress from her busy life.
As the days progressed, she began to feel she was falling apart. Strange symptoms surfaced—numbness in her feet, and bizarre sensations. Something was wrong.
Doctors offered explanations but no real answers. MRIs revealed mysterious lesions on her brain, attributed casually to normal aging. A CAT scan uncovered a tumor on her adrenal gland, prompting surgery that only briefly masked the underlying cause.
Amy felt trapped in a maze of misdiagnoses, each step leading deeper into confusion. Her health worsened—seizures, hallucinations, and frightening episodes of blood sugar crashes. Still, her doctors remained baffled.
What about Lyme disease?
Determined, Amy embarked on her own research. She stumbled on a condition eerily matching her symptoms—Lyme disease. Yet initial tests were negative, and doctors were skeptical.
Unwilling to surrender, she found a Lyme specialist. Rigorous testing followed, and finally, the mystery unraveled. Two positive tests confirmed what Amy had suspected: Lyme disease from that forgotten summer bite, overlooked for years.
Tan’s battle wasn’t over—the treatments were difficult, costly, and sometimes debilitating—but the clarity of knowing provided the strength she needed. Amy Tan had solved her own medical mystery.
Amy Tan’s story is one of a physical disease missed by physicians who did not recognize Lyme disease as the underlying cause. In fact, numerous physical diseases—from infections to endocrine imbalances—can masquerade convincingly as emotional problems.
Misdiagnosis may result in incorrect treatments, prolonged suffering, and, in the worst cases, deaths. This means that it is critical to differentiate true psychological conditions alone from symptoms triggered by an underlying illness. At times, the patient can aid in this investigation.
Mental health symptoms of physical diseases
Parkinson’s Disease: Known for tremors and rigidity, Parkinson’s can also hide emotional disturbances such as depression, anxiety, impulse control issues, and even psychosis, often before any movement problems appear. Ironically, medications for motor symptoms might worsen anxiety.
Coronary Artery Disease and Heart Attacks: Anxiety and depression commonly accompany heart troubles. After a heart attack, up to half of patients experience anxiety, while about one in five faces significant depression.
Pulmonary Embolism: A sudden blockage in the lung’s artery can provoke intense anxiety and fear, mimicking panic attacks. Survivors may grapple with ongoing anxiety and depression.
Seizure Disorders: A specific kind of seizure, Complex partial seizures, emanating from the brain’s temporal lobe, often look like psychiatric disorders due to their emotional, cognitive, and behavioral symptoms. Misdiagnosis can lead to severe health consequences.
Hypoglycemia (Low Blood Sugar): Low blood sugar causes confusion, anxiety, irritability, and altered consciousness, easily mistaken for psychiatric or neurological disorders.
Adrenal Disorders:
- Pheochromocytoma: This adrenal tumor releases adrenaline-like hormones, causing episodes of anxiety, rapid heartbeat, and sweating that closely resemble panic attacks.
- Cushing’s Syndrome: High cortisol levels trigger anxiety, depression, and cognitive impairment, often resolving once cortisol normalizes.
- Encephalitis: Brain inflammation, often autoimmune or infectious, can cause dramatic changes like psychosis, obsessive behaviors, or cognitive dysfunction, sometimes mistaken for severe psychiatric disorders.
Neurosyphilis: Once a common cause of psychiatric hospitalization, neurosyphilis can provoke psychosis, memory loss, and personality changes. Though treatable, recovery from psychiatric symptoms is unpredictable.
Huntington’s Disease: This inherited neurological condition typically brings depression, anxiety, hostility, and psychosis before its characteristic movement disorders appear.
Carcinoid Tumors: These gastrointestinal tumors produce serotonin, causing anxiety, abdominal pain, flushing, and diarrhea, significantly impacting patients’ emotional well-being.
B12 Deficiency: Lacking Vitamin B12 may cause depression, psychosis, ADHD-like symptoms, or obsessive-compulsive behaviors. Supplementation often dramatically reverses symptoms.
Thyroid Disorders:
- Hyperthyroidism: Excess thyroid hormones can stimulate aggression, anxiety, mania, and psychosis.
- Hypothyroidism: Deficient thyroid function can lead to severe depression, cognitive slowing, or even “myxedema madness,” a psychotic condition reversible with hormone treatment.
Hypercalcemia: Elevated calcium levels can dull thinking, provoke confusion, or lead to severe mental status changes, resolving once calcium returns to normal.
Substances: Recreational and prescription drugs—like alcohol, cocaine, ketamine, ecstasy, benzodiazepines, PCP, or even antihistamines—can mimic psychiatric symptoms, emphasizing the importance of careful screening for substance use or withdrawal.
Summary
What initially seems like purely psychological trouble may indeed have roots in physical conditions that, once identified, can often be successfully treated.
Shirley M. Mueller, M.D., is a neuroscientist board certified in neurology and psychiatry. She is also an avid collector. Combining these two disciplines, she wrote Inside the Head of a Collector: Neuropsychological Forces at Play. This article originally appeared in Psychology Today.















