O ne night years ago, when my daughter was at her sickest, she asked me, “Is the chandelier hanging sideways?” With a curious look on my face, I answered, “No. Why?”

She said everything in the room, including the walls, looked tilted, like she was in Whoville, the town in Dr. Seuss’s book Horton Hears a Who!
A month later, a prestigious children’s hospital diagnosed her with myalgic encelphalomyelitis (ME) and chronic fatigue syndrome (CFS). The doctors gave no other explanation for her laundry list of symptoms, including a recurring fever.
Little did we know that she had a raging infection inside her brain. Her nightly visits to Whoville continued for months. They finally stopped, after she was diagnosed with neurological Lyme disease and co-infections and treated with antibiotics.
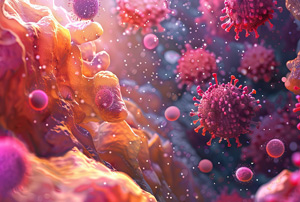
Patients with late-stage Lyme are no strangers to the neurological manifestations of this illness. Symptoms like brain fog, anxiety, depression, and insomnia are common complaints in this population. But what causes all these symptoms? Inflammation. Like in many other illnesses, inflammation is the enemy.
At ILADS 2019, Dr. Tania Dempsey emphasized the importance of diagnosing and treating mast cell activation syndrome when it is suspected in the course of Lyme disease.
Mast cells are a complicated aspect of our immune system. When mast cells go haywire, they cause inflammation. (I’ve written extensively about mast cell diagnosis, treatment, and how it helped solve the puzzle of my daughter’s illness.) Dr. Dempsey has found that incorporating mast cell treatment into her Lyme protocols helps to reduce many of the symptoms of “Lyme brain” by controlling inflammation. In my daughter’s case, finding the right mast cell protocol was a critical step in getting her into remission.
Disseminated Neurological Lyme Disease
Neurological Lyme disease symptoms are largely invisible and difficult to quantify. Thus, many physicians write them off as psychosomatic, leaving these patients with no validation or treatment options…….Join or login below to continue reading.