Steven Harris, MD, is a board-certified family practitioner with a focus on chronic, complex illnesses including Lyme disease and associated tick-borne infections. As part of the Bay Area Lyme Foundation’s Distinguished Speaker Series, he recently spoke on “Treating Complex Chronic Diseases: Novel Therapeutic Options for Lyme Patients.” In his talk, he discussed wide-ranging topics including precision medicine, mitochondrial function, regenerative medicine, body alignment and toxic loads. Below is a transcript of his presentation.
Steven Harris, MD, is a board-certified family practitioner with a focus on chronic, complex illnesses including Lyme disease and associated tick-borne infections. As part of the Bay Area Lyme Foundation’s Distinguished Speaker Series, he recently spoke on “Treating Complex Chronic Diseases: Novel Therapeutic Options for Lyme Patients.” In his talk, he discussed wide-ranging topics including precision medicine, mitochondrial function, regenerative medicine, body alignment and toxic loads. Below is a transcript of his presentation.
What is “Precision Medicine”?
T he concept of precision medicine, which is a growing area, is where we look at an individual and try to create a tailored plan for that person. I think many doctors wish that we could have a ‘cookbook’ approach to medicine that would work for our patients. But unfortunately, that approach doesn’t work.
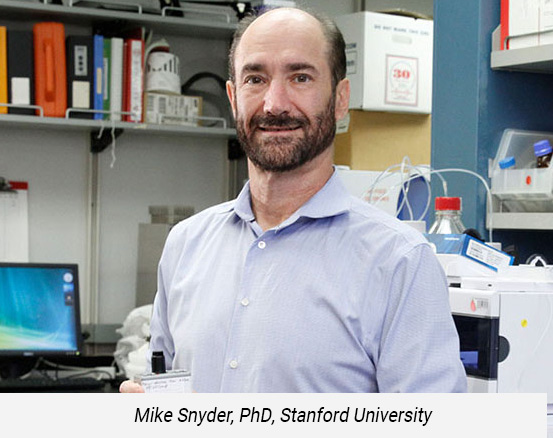 Luckily, here in the San Francisco Bay Area, there are doctors offering precision medicine including Dr. Sunjya Schweig in Berkeley, Dr. Christine Green, with us at Pacific Frontier Medical, and Dr. Eric Gordon, at Gordon Medical Associates in Marin and others. And thankfully, we have Stanford and UCSF (our local medical centers) that we work peripherally with. In addition, the Open Medicine Foundation is making great strides in understanding illness and Dr. Mike Snyder’s group at Stanford who are working on multiomics for chronic fatigue that track an individual patient’s data.
Luckily, here in the San Francisco Bay Area, there are doctors offering precision medicine including Dr. Sunjya Schweig in Berkeley, Dr. Christine Green, with us at Pacific Frontier Medical, and Dr. Eric Gordon, at Gordon Medical Associates in Marin and others. And thankfully, we have Stanford and UCSF (our local medical centers) that we work peripherally with. In addition, the Open Medicine Foundation is making great strides in understanding illness and Dr. Mike Snyder’s group at Stanford who are working on multiomics for chronic fatigue that track an individual patient’s data.
These doctors are working in their own fields, not necessarily just tick-borne diseases, but our work overlaps. For example, the Snyder Lab multiomic study involves genomics, epigenomics, metabolomics, where they are looking at tons of data and assimilating a lot of this different data to try to create treatment plans that work for the individual, because of the fact that a ‘cookbook’ approach doesn’t work for this group of chronic complex patients.
For example, we look at someone’s multiome and the parts that make them up, including their microbiome, epigenome among many others, which is becoming a bigger and more exciting field. One of the practical aspects we try to determine is how to address an individual’s level of inflammation, the diversity of their personal bacterial flora, and how to help compensate for any deficiencies — or over abundances — that help contribute to disease.
Precision medicine doctors are looking at as much data as we can, but we are also learning to incorporate treatments that illustrate how our bodies interact with an ever more toxic world, such as with glyphosate and organophosphates, toxic metals, among hundreds of others harmful agents. Some may argue that electromagnetic sensitivity or electromagnetic stressors are also affecting people. This needs more research and is still a very young field, but what providers report is that electromagnetic sensitivity does affect many patients. In addition, if we look at some of the old stalwarts, such as mold, actinomyces, and other biotoxins, these can contribute significantly to a patient’s burden of illness. So, taking a very detailed approach to looking at what external stressors someone has is really important.
Human Energy and Mitochondrial Function
 Another nascent area that is probably going to become bigger is mitochondrial work, i.e., mitochondrial function — at least in the ME/CFS world — which translates too many other areas, including the Lyme and co-infection world, because illness and wellness is fundamentally all about energy.
Another nascent area that is probably going to become bigger is mitochondrial work, i.e., mitochondrial function — at least in the ME/CFS world — which translates too many other areas, including the Lyme and co-infection world, because illness and wellness is fundamentally all about energy.
The concept is that if we have enough energy to mobilize our immune systems and get ourselves to detoxify, and to absorb nutrients, the body will be able to function effectively on its own. The goal of treatment is to ease the body to do what it needs to do by itself without so much external intervention. That is one of the subtle things that we’re learning as we do this. The approach in the past has been, ‘there’s an infection and we want to knock the infection out,’ but many times we have discovered that healing doesn’t work that way.
 Dr. Eric Gordon describes the healing exchange as being like a dance that the provider helps the patient do with various treatments. You try to tease out the way forward to get on the right path, like finding that yellow brick road. And if we are able to do that leg work early on to eliminate the stressors, evaluate and optimize the mitochondrial dysfunction, etc., then we can often take a much more direct path to wellness.
Dr. Eric Gordon describes the healing exchange as being like a dance that the provider helps the patient do with various treatments. You try to tease out the way forward to get on the right path, like finding that yellow brick road. And if we are able to do that leg work early on to eliminate the stressors, evaluate and optimize the mitochondrial dysfunction, etc., then we can often take a much more direct path to wellness.
What is exciting is that there are new tests in the research world that assess mitochondrial function. Seahorse testing, for example, currently in the research phase, looks at ATP production and free phosphate production. We’ve been using mitochondrial muscle biopsies primarily to evaluate mitochondria in the past, but there’s more to investigate regarding the way energy is made at a cellular level. In the near future more research is going to be examining the inner mitochondrial membrane to watch how the very basic pieces of electron chemistry are translating to a cell and then translating to the organism as a whole.
Telomeres and Cellular Aging
 Dr. Horvath and a group at Stanford recently wrote a paper focused on decreasing cellular aging using things like growth hormone and DHEA, and metformin (a diabetes drug), to try to decrease the age of cells. There’s also a lot of talk in medical fields about telomeres and their relationship with cellular senescence. The hard part is, how do we translate this when a patient comes into the office and put burgeoning research into actual practice? Much of this is not going to be FDA approved as treatments for perhaps the next 10 or 15 years. So, part of the approach to addressing some of these very complicated patients is working in a partnership with them, because we don’t have the answers. We can work towards the likely answers, but sometimes we have to do it with very short steps, and with a patient who is deeply engaged in the treatment process.
Dr. Horvath and a group at Stanford recently wrote a paper focused on decreasing cellular aging using things like growth hormone and DHEA, and metformin (a diabetes drug), to try to decrease the age of cells. There’s also a lot of talk in medical fields about telomeres and their relationship with cellular senescence. The hard part is, how do we translate this when a patient comes into the office and put burgeoning research into actual practice? Much of this is not going to be FDA approved as treatments for perhaps the next 10 or 15 years. So, part of the approach to addressing some of these very complicated patients is working in a partnership with them, because we don’t have the answers. We can work towards the likely answers, but sometimes we have to do it with very short steps, and with a patient who is deeply engaged in the treatment process.
“It’s like a dance that the provider helps the patient do with various treatments. You try to tease out the way forward to get on the right path, like finding that yellow brick road.”
This is a very different model than we’re used to. When I grew up, the doctor told you what treatments to take. You took the treatment. Then, you went back and reported your symptoms. This doesn’t seem to work for this very complicated group of patients. These patients also happen to be some of the most savvy, educated, well-researched, intelligent people, mostly because they’ve been through so much and have seen so many doctors. By the time they come to one of us, they may have seen 20 or 30 doctors. So, we have to offer them something fresh and new that also has a high likelihood of actually working.
 On top of the physical issues, we must also consider the psychological burden that chronic illness has had on people. This may seem simple and obvious, but it is such an important piece: We have to address the trauma. And sometimes we can’t address trauma head on. We have to address it in a very circuitous but meaningful way. There are a lot of non-pharmacological, non-ingestible ways to do this: Through the Dynamic Neural Retraining SystemTM (DNRS), through vagus nerve training, through neurofeedback, neuro stimulation, and through various other methods.
On top of the physical issues, we must also consider the psychological burden that chronic illness has had on people. This may seem simple and obvious, but it is such an important piece: We have to address the trauma. And sometimes we can’t address trauma head on. We have to address it in a very circuitous but meaningful way. There are a lot of non-pharmacological, non-ingestible ways to do this: Through the Dynamic Neural Retraining SystemTM (DNRS), through vagus nerve training, through neurofeedback, neuro stimulation, and through various other methods.
There is a new device called the PoNS device, which will hopefully become widely available very soon, which is a tongue neurostimulation device. It is FDA approved for head trauma, but it also works for post-traumatic stress disorder. It’s an amazing way to use electricity with neuro signaling to the amygdala and help to retrain the brain to get out of that stress response. A scientist in Wisconsin, Yuri Danilov, developed it and the company that owns it is called Helius Medical technologies. They’re trying to get FDA approval for it, and they are making it available to physical therapists. It’s mentioned in Dr. Norman Doidge’s book The Brain’s Way of Healing. I’ve seen it used with some patients, and it’s phenomenal.
Regenerative Therapies and Exosomes
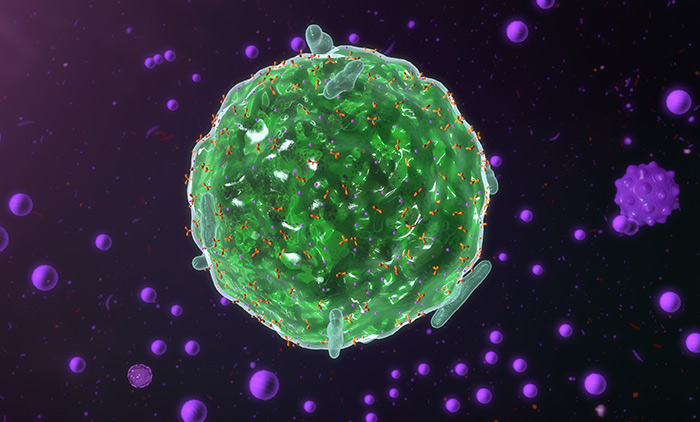
 In addition to the cell aging and telomere lengthening concept, one area that does seem to be slightly farther ahead is the field of regenerative therapies. Regenerative therapies include exosomes, PRP, and alpha 2-macroglobulin, among others. Some of these chemicals are injected. Oftentimes, we use it mostly for tendon issues and for osteoarthritis and for different orthopedic situations. But exosomes, especially, have other uses. There are many doctors who are using exosomes in parallel to stem cell therapies and there are many types of stem cells from autologous cells that come from your own body—to umbilical, to fetal, all the way to human embryonic.
In addition to the cell aging and telomere lengthening concept, one area that does seem to be slightly farther ahead is the field of regenerative therapies. Regenerative therapies include exosomes, PRP, and alpha 2-macroglobulin, among others. Some of these chemicals are injected. Oftentimes, we use it mostly for tendon issues and for osteoarthritis and for different orthopedic situations. But exosomes, especially, have other uses. There are many doctors who are using exosomes in parallel to stem cell therapies and there are many types of stem cells from autologous cells that come from your own body—to umbilical, to fetal, all the way to human embryonic.
There is a book by Amy Scher titled, This is How I Save My Life. She has become a notable author who wrote about her journey through India, where she received human embryonic stem cells, and went from a very severe neurologic case of Lyme to being quite well now.
“When I grew up, the doctor told you what treatments to take. You took the treatment. Then, you went back and reported your symptoms. This doesn’t seem to work for this very complicated group of patients. “
These various therapies can be amazing if used properly, but we need more studies. Much of this is outside of the purview of many mainstream practitioners and health plans and the medical establishment at large. But many of these treatment approaches can be done safely and effectively, and definitely have their place for decreasing that overall illness burden.
 One of the thoughts about stem cells used to be that ‘Oh, the stem cells can change into whatever cell, and then the cells can regenerate this way or that way.’ But what we now think is that it’s probably more to do with the cell signaling chemicals, and the growth factors, that are really at play here. Exosomes don’t have any nucleic acid in them, it’s just those chemicals themselves. Many people are using those very successfully and it’s still early, obviously, but there are some very neat ways to do it, especially with some of the structural conditions such as CCI.
One of the thoughts about stem cells used to be that ‘Oh, the stem cells can change into whatever cell, and then the cells can regenerate this way or that way.’ But what we now think is that it’s probably more to do with the cell signaling chemicals, and the growth factors, that are really at play here. Exosomes don’t have any nucleic acid in them, it’s just those chemicals themselves. Many people are using those very successfully and it’s still early, obviously, but there are some very neat ways to do it, especially with some of the structural conditions such as CCI.
The Body’s Structure and Craniocervical Instability
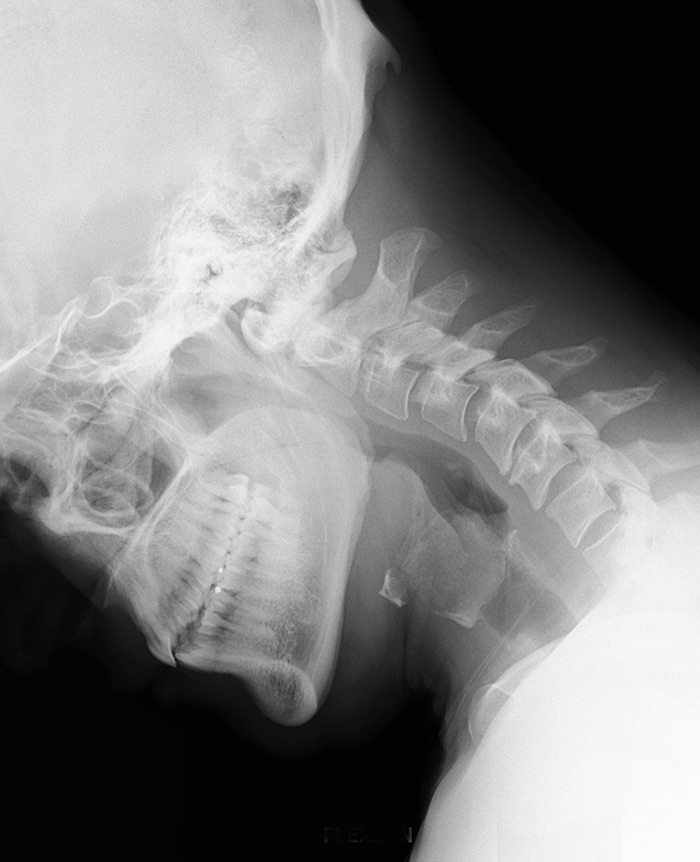 CCI is Craniocervical Instability, which is a fairly new conceptual understanding, but as a condition it’s been with us for a long time. It is where micro shear forces are happening in the neurovascularly structurally dense area where the skull meets the cervical spine, which can lead to lots of inflammatory responses. Mast cells, which are some of the allergy producing cells, are involved, among many other immune cells.
CCI is Craniocervical Instability, which is a fairly new conceptual understanding, but as a condition it’s been with us for a long time. It is where micro shear forces are happening in the neurovascularly structurally dense area where the skull meets the cervical spine, which can lead to lots of inflammatory responses. Mast cells, which are some of the allergy producing cells, are involved, among many other immune cells.
A very big inflammatory response occurs when there is a combination of an infection, such as Borrelia, Babesia or Bartonella, mycoplasma, viruses, et cetera, usually plus head trauma, or a hypermobility syndrome such as Ehlers-Danlos; it’s one of the part of a triad for these people who are a setup for CCI. Dr. David Kaufman is an expert in the area who helped popularize the idea of CCI, and it’s been absolutely amazing for some of these patients who have especially severe chronic fatigue. The ME/CFS world are early adopters in considering it, but for many Lyme patients and practitioners, it is not yet on their radar.
It should be because fatigue is one of the very significant presentations of chronic Lyme patients. I’ve seen four or five patients who have had this surgery with pretty astounding results. But what we’re trying to do is get away from a fusion surgery if at all possible. That’s where the exosomes can theoretically come in, especially properly placed injections of exosomes and PRP and these other regenerative therapies to stabilize an area in the cervical spine. The inflammation goes down with many of these injections but getting the benefits to continue when people move their heads frequently is another matter.
“Much of this is outside of the purview of many mainstream practitioners and health plans and the medical establishment at large. But many of these treatment approaches can be done safely and effectively, and definitely have their place for decreasing that overall illness burden.”
Obviously, this is a complicated and very new field, and the challenge is that the neurosurgery boards in America don’t allow surgery for fatigue. You need something like a chiari malformation or an instance where a vital system is being compromised before the neurosurgeon can actually do surgery for this. So, sometimes by the time they do surgery, the patient can be significantly decompensated. The results aren’t quite as good as they would have been if we could have done it earlier. But in addition to the environment, genomics, and metabolomics, and microbiome, a way to approach some of these pathogens is by looking at a patient’s body structure — CCI being one of those aspects.
Jaw Misalignment, CCI and Spinal Issues
Another important structural approach is to investigate jaw misalignment. We can see when people have a bite that’s ‘off.’ There’s been quite a bit of work on this, mostly with the craniosacral folks, but there’s some very good science that shows that every time we speak, and every time we bite that we’re moving our cerebral spinal fluid, and if it moves and flows in an aberrant way, then the whole nervous system becomes ‘off’ as it were.
Sometimes just by repositioning the jaw we can make an incredible impact on patients. I’ve seen absolute magic. It’s not usually something we do first, but it is something that we now think about, especially with the chronic complex illness. We look at things like root canals, and of course, that’s old news, but it’s still important looking at some areas of surgery and surgical scars and things like titanium rods, etc.
“One insult by itself isn’t probably going to do anything. Throw that insult in with the Lyme, with the environment, with the structural issues, and you start seeing how complicated some of these patients are.”
Therefore, jaw misalignment along with CCI and other spinal issues, such as scoliosis and different ways the spine presents in space can have very profound implications for a chronic illness. Let’s not forget, these patients are coming to me, and they typically also have infections. So, the infections are probably one of those rate-limiting steps. There are a lot of people who have scoliosis and who have jaw misalignment and CCI, who aren’t actually sick. But when you throw in what these infections are doing to people, and you combine that with the structural issues, then you start seeing the picture come together about the infections.
 And it’s not just about Lyme and babesia species and Bartonella and ehrlichia and anaplasma, relapsing fever, borrelia, etc. There are a lot of other organisms that come into play: there are a lot of GI parasites, brain parasites, worms, and amoebas of all kinds that compromise the human system. Not that they’re necessarily making people sick by themselves, but they change the conditions in the body. One insult by itself isn’t probably going to do anything. Throw that insult in with the Lyme, with the environment, with the structural issues, and you start seeing how complicated some of these patients are.
And it’s not just about Lyme and babesia species and Bartonella and ehrlichia and anaplasma, relapsing fever, borrelia, etc. There are a lot of other organisms that come into play: there are a lot of GI parasites, brain parasites, worms, and amoebas of all kinds that compromise the human system. Not that they’re necessarily making people sick by themselves, but they change the conditions in the body. One insult by itself isn’t probably going to do anything. Throw that insult in with the Lyme, with the environment, with the structural issues, and you start seeing how complicated some of these patients are.
And so, then it becomes a question of, ‘Okay, let’s evaluate all these different things that could be happening.’ I look at it as being like an onion. What’s the top layer of the onion? How do you pull that top layer off and then go to the next one and then finally get to the core? It’s a model that often works. It’s just sometimes slow, but it’s better to be slow and complete than trying to race to the finish and then having to do it over again.
Viruses and Body Decompensation
 And then of course viruses are another piece of the puzzle, that are becoming bigger and bigger. We just happen to be right in the midst of a very large viral thing right now. Viruses have their own problems, and they can cause the body to decompensate on its own. But in the case of things like Epstein Barr and human herpesvirus 6, enteroviruses and varicella, they can be very opportunistic. We know about opportunistic viruses through the HIV world.
And then of course viruses are another piece of the puzzle, that are becoming bigger and bigger. We just happen to be right in the midst of a very large viral thing right now. Viruses have their own problems, and they can cause the body to decompensate on its own. But in the case of things like Epstein Barr and human herpesvirus 6, enteroviruses and varicella, they can be very opportunistic. We know about opportunistic viruses through the HIV world.
The immune system is typically able to surveil these opportunistic infections really well. However, if the body becomes weakened, whether through the immune system already being weak or there’re being too many stressors on it, those viruses can take on a life of their own.
Dr. Jose Montoya earlier and now the current folks at Stanford in the chronic fatigue center are looking closely at human herpesvirus 6. The late, great Paul Cheney, who was so important in putting chronic fatigue on the map, was looking at human herpesvirus 6 primarily, while John Chia has been very involved with enteroviruses. These different viruses definitely can contribute to fatigue and contribute to various related symptoms. But, in my view, they are often purely opportunistic and come up because the body is decompensated. So just treating those, in my experience, hasn’t been fully effective, but it is very important to look at them in the overall scheme of what we’re doing for patients.
mTOR Agents and Autophagy
 At an ILADS conference a few years back, Dr. Steven Phillips did an amazing talk on the use of mTOR agents, (mammalian target of Rapamycin). This process has to do with how our cells can clean the body by degrading older and dead cells. People who can clean their body of debris have a much higher chance to heal and recover. People who have high levels of autophagy can heal, because there’s cellular turnover and new healthy cells taking the place of old or unruly cells.
At an ILADS conference a few years back, Dr. Steven Phillips did an amazing talk on the use of mTOR agents, (mammalian target of Rapamycin). This process has to do with how our cells can clean the body by degrading older and dead cells. People who can clean their body of debris have a much higher chance to heal and recover. People who have high levels of autophagy can heal, because there’s cellular turnover and new healthy cells taking the place of old or unruly cells.
There are many agents that we’re starting to look at for people who have been sluggish, who have been sick for many years, and have been through many different treatments and have been stagnant. Trying to increase one’s autophagy through the use of things like Rapamycin is starting to get attention nationwide. At the 2022 ILADS conference in Orlando, I met with many people who are starting to use this cancer drug in low doses to try to increase the body’s ability to rid itself of debris. Other things include Honokiol, which is a magnolia leaf, and doxycycline, and many other agents increase autophagy including methylene blue. This is one of those areas that we’re exploring as a group, and one of the ways that we approach these complicated patients. Vitamin D is another example of an mTOR agent.
“If the body becomes weakened, whether through the immune system already being weak or there’re being too many stressors on it, those viruses can take on a life of their own.”
Toxic Load, Nutrient Status and Environmental Stressors
One way to approach patients is to look at what’s happening with their ability to absorb nutrients and then get rid of waste i.e., absorption and detox. And it always comes back to that for many of us in the day-to-day working with these patients: how do we increase their absorption and nutrients? Their ability to tolerate nutrients? Their ability to get rid of the stuff that they don’t need? One way to do that is through membrane chemistry and using different kinds of fats to flush out some of the debris, on the so-called classic lipid bilayer on the surface of cells.
There were common, simple methods used in the past to just detox patients and assist them in draining and elimination that we used to employ, but simple strategies no longer work in the most complex subset of patients. Oftentimes there is too much happening in their metabolism. There’s too much junk that is causing their bodies to react. Sometimes the reactivity is so profound that nothing happens if we can’t fix that reactivity.
 Sometimes, this over reactivity is related to infection. Sometimes it’s because there’s too many bad chemicals in the body. With all of these environmental exposures that people have, a way for the body to respond to these stressors is by overreacting. While it could be driven by just the infections, it’s usually a complicated causation as to why people have ‘mast cell activation.’
Sometimes, this over reactivity is related to infection. Sometimes it’s because there’s too many bad chemicals in the body. With all of these environmental exposures that people have, a way for the body to respond to these stressors is by overreacting. While it could be driven by just the infections, it’s usually a complicated causation as to why people have ‘mast cell activation.’
We learned about it through a tumor of mast cells called mastocytosis. This is a little bit different because people don’t have these tumors, but they elicit an infection-related, allergy-producing response. It’s the body trying to help itself, but it does so ineffectively and in a way that increases a person’s suffering.
David Kaufman and some other folks have found a triad of Ehlers-Danlos or hypermobility syndrome with what’s called POTS or orthostatic tachycardia with mast cell activation. We’re finding groups of these people where this hypersensitivity syndrome is actually the first thing that we have to assess. Unless that is successful the rest of the treatment process can’t really ensue.
Again, we used to just do some detox, get patients prepared, and then work from the top down, working on the biggest thing like worms, then go to parasites, then go to metals, then go to babesia, then go to Lyme, etc. Now that initial dance to diminish the reactivity can become the bulk of the treatment regime. On the positive side, once we get past that part, the rest of the treatments can often be done faster, with very positive results, where patients develop momentum in approaching wellness.
“In conclusion, these are a few different ways to address this most complicated, most difficult group of patients. I truly believe that everybody can get better, and I think that sharing that hope with the patient is a way for them to be able to hold on during what is a marathon for many of them. Not everybody needs to take every step, but the steps are there, and it can be done.” — Dr. Steven Harris
This transcript is republished with permission from the Bay Area Lyme Foundation. Editor’s note: Any medical information included is based on a personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.