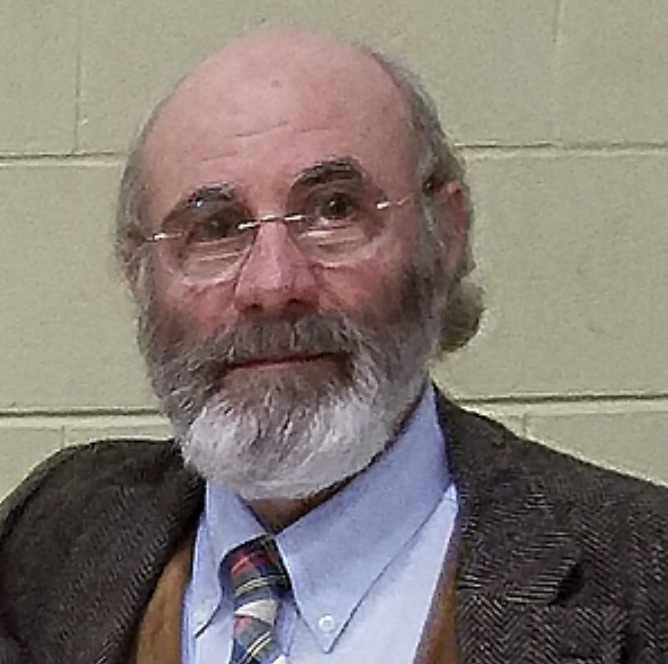
 K enneth Liegner, MD, has been on the frontlines of treating Lyme and other tick-borne diseases for more than thirty years. Recently, author Dana Parish interviewed him on the Bay Area Lyme Foundation’s Ticktective™ podcast.
K enneth Liegner, MD, has been on the frontlines of treating Lyme and other tick-borne diseases for more than thirty years. Recently, author Dana Parish interviewed him on the Bay Area Lyme Foundation’s Ticktective™ podcast.
Their conversation addressed many topics, including the history of Lyme disease in the US and the lack of recognition of the illness among clinicians, the government, and insurance companies. They talked about the treatment challenges of co-infections like babesiosis, and touched on how a COVID infection may impact Lyme patients, causing a recurrence of latent symptoms. And they discuss Dr. Liegner’s pioneering use of disulfiram—a drug initially used to treat alcoholism—as an off-label therapeutic for his Lyme patients.
The following is a transcript of an excerpt of the podcast interview.
- QDana Parish: You were a pioneer in discovering disulfiram for the treatment of Lyme disease. How did you come upon that, and how did it go? It’s been a couple years now, so what do you think now?
-
AKenneth Liegner: Well, I can’t take credit for discovering it for its utility in Lyme. It was the work of Jayakumar Rajadas. I was the first clinician to apply it in patients. Jayakumar Rajadas and his coworkers at Stanford did some high throughput testing of thousands of compounds and just tested them to see which had activity against the Lyme spirochete. And it turned out that disulfiram was way up there at the top, or near the top, if not at the top, having activity way more than doxycycline/Rocephin. So, that was published in an article in a little bit of an obscure journal, and nobody really paid all that much attention to it. Then at the first Lyme Mind Conference that was held at Mount Sinai sponsored by The Steven & Alexandra Cohen Foundation, they really got some great people together. The keynote speaker for that conference was Kim Lewis, who’s from Northeastern (University).
Towards the end of his talk, he mentioned Rajadas’ work, and that disulfiram had this huge activity. One of my patients had been following Kim Lewis’s work and it (the keynote speech) was later posted on YouTube. This is a patient I’d worked with for quite a few years, very trustworthy. He was kept pretty well on a regimen of amoxicillin, minocycline, and malarone. But if he went off treatment, he would deteriorate. He saw this presentation, and he told me about it.
“And if you’re going to use it, you have to be really familiar with the drug, and you have to follow the patients carefully. Even today, we’re still trying to figure out different ways in which it can be used.”
So, I viewed it, and I was already familiar with the paper. I reread it. I’d never used disulfiram because I just had no occasion to use it. It is a drug that has been used mainly for treating alcoholism, which is not my field. I knew that it existed, but I had never used it. I looked it up at the patient’s request. I never would’ve suggested it to the patient. The patient asked if I would let him try it. Now, it’s a drug that’s been used for decades and is generally safe. And although it does have some potential toxicities, I allowed him to try it. And it’s a long, long story. It’s outlined in the articles that were published. There was the first article about the first three patients published in MDPI antibiotics. Then we published another paper a little bit later reporting on our experience with another 60 or 70 patients.
The first 3 patients that we used it on, bing! bing! bing! It was a dramatic improvement. And these are tough cases. These are not easy cases. That influenced me to publish on it. And of course, with that, it has gotten a lot of attention. It is a drug that has to be used with care. And it’s not something I just throw at people willy-nilly. It’s got to be the right person in the right way. And if you’re going to use it, you have to be really familiar with the drug, and you have to follow the patients carefully. Even today, we’re still trying to figure out different ways in which it can be used.
- QDana Parish: It occurs to me it should not be the first line of defense against Lyme.
-
AKenneth Liegner: I’m not using it that way. I’m not using it as a first line. First of all, it’s still relatively new. I would not say it’s, quote, ‘the standard of care,’ you know?
- QDana Parish: Is it getting people durably better? Now that you’ve had a couple years with it, are there patients that have gotten well with it, that were intractable before and now don’t need to come see you every three or six months anymore?
-
AKenneth Liegner: Yes. But I don’t ever tell them to expect it. Nor do I declare that they are, quote, ‘cured.’ Because I don’t know. All I know is that there’s a subset of those who are treated, but not everybody who seems to get substantially better or well, and where they don’t need to see me for years at a time. So, I think it’s very potent. But again, it has certain toxicities that can be quite serious, even fatal, or resulting in irreversible neurologic injury. So, you have to be judicious with who you use it with. People need to be fully informed. As a clinician, you are obliged to follow them carefully and be vigilant. Usually with some of these complications if you recognize it, you need to stop the drug. And usually, those adverse reactions will reverse. But even then, you can’t say that. You don’t always know that they’re going to reverse. So, it’s tricky. It’s potent, but it has to be used with care, judiciously.
- QDana Parish: I’ve heard some really remarkable stories for sure, some remarkable recovery stories. Early on, when you were first using it, people that were languishing for years, trying different things, were finally improving.
-
AKenneth Liegner: The thing about it is, it’s as cheap as borscht! I mean, relatively speaking, compared to intravenous Rocephin, which is expensive and inconvenient. It also has risks. To me, it’s just another tool in the toolbox. And you can’t have too many tools. We need more tools in the toolbox.
- QDana Parish: But it’s great that you found that, and it’s helped a subset of your patients and other people have gone on and adopted it and have helped some of their patients. We need more innovation of course. But thank you for that. What my hope is now is that all this Long Covid research will inform chronic Lyme. Do you think that might happen? Is there hope on the horizon for chronic Lyme patients? In light of all the awareness now of what a chronic common infection can do?
-
AKenneth Liegner: I think there’s going to be some synergy there. But I think really in order to solve the problem, you need to acknowledge it for what it is. And that’s why I reiterate it’s important to acknowledge chronic Lyme, the infection. There can be other elements, like neuro autoimmune components for sure. Or maybe even post-infections in some people. But for many people it’s the infection. And if you don’t acknowledge that, then your research for treatment is going to be misaligned. You need to find a way to definitively deal with the infection. And of course, the hope and the goal would be to find something that’s absolutely curative, that eliminates the infection completely—unless you get reinfected—that should be the goal. That should be where the effort should be directed. Also, the other thing that’s important is to have a definitive direct detection test that’s qualitative, as well as semi-quantitative, that can help us to know the status of the infection and also the response to treatment in an objective way. That’s been lacking.
- QDana Parish: Absolutely. I love this quote. It’s your quote. I remember the first time I read it, I almost fell off my chair because it just says it all. So, I’m going to read it. You said, “In the fullness of time, the mainstream handling of chronic Lyme disease will be viewed as one of the most shameful episodes in the history of medicine. Because elements of academic medicine, elements of government, and virtually the entire insurance industry have colluded to deny a disease.” If that just doesn’t say it all. Nobody could say it better than that. That’s just the truth.
“In the fullness of time, the mainstream handling of chronic Lyme disease will be viewed as one of the most shameful episodes in the history of medicine. Because elements of academic medicine, elements of government, and virtually the entire insurance industry have colluded to deny a disease.”
Editor’s note: Any medical information included is based on a personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.