E njoying the outdoors can put you in contact with more ticks, and with them greater – and growing – risk of Lyme disease.
E njoying the outdoors can put you in contact with more ticks, and with them greater – and growing – risk of Lyme disease.
Between 2007 and 2021, insurance claims involving Lyme have increased by 65% in urban areas and by more than 350% in rural areas, according to FAIR Health. And the federal Centers for Disease Control and Prevention now estimates that nearly half a million people in the U.S. contract Lyme disease every year.
Of these, 10% to 15% may develop post-treatment Lyme disease syndrome, which can be thought of the way we think about long COVID.
“Long Lyme” causes persistent symptoms even after appropriate antibiotic treatment for Lyme disease.
But lack of alignment and agreement among physicians and public health authorities about Lyme diagnosis and treatment and what constitutes post-Lyme – as well as limited clinical understanding and diagnostic availability – has left a growing number of patients without the support and help they need.
Similarities between “long Lyme” and “long COVID”
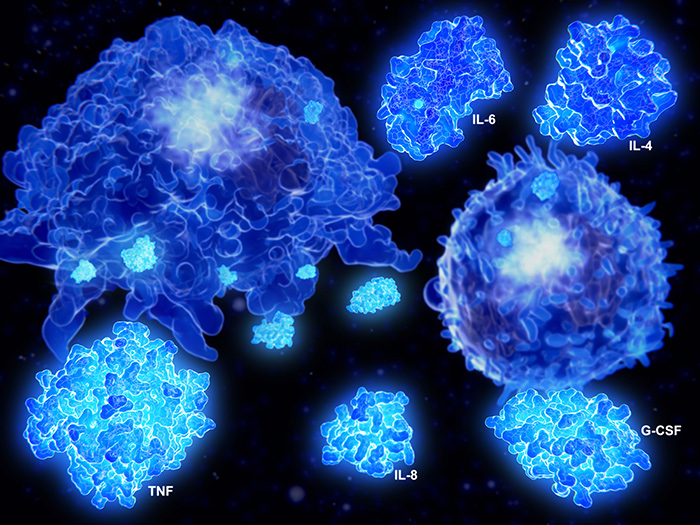 Making matters worse, post-Lyme (and, for that matter, long COVID) may not be caused by persistent infection, but instead by overactive immune response to proteins left in the body after infection. And symptoms of these diseases, including fatigue, brain fog and exhaustion after exercise or exertion, are very similar if not identical to one another, and to chronic fatigue syndrome.
Making matters worse, post-Lyme (and, for that matter, long COVID) may not be caused by persistent infection, but instead by overactive immune response to proteins left in the body after infection. And symptoms of these diseases, including fatigue, brain fog and exhaustion after exercise or exertion, are very similar if not identical to one another, and to chronic fatigue syndrome.
Another confounding factor in chronic inflammatory conditions such as post-Lyme and long COVID is mental health symptoms most likely caused by neuroinflammation, an inflammatory response within the brain or spinal cord. Standardized and objective definitions that separate distinctly different physiological causes can help……….Join or login below to continue reading.