Ehrlichiosis — the Tick-Borne Disease No One Has Heard Of While some cases of ehrlichiosis are mild, the disease can be severe or fatal if not treated correctly, even in previously healthy people.
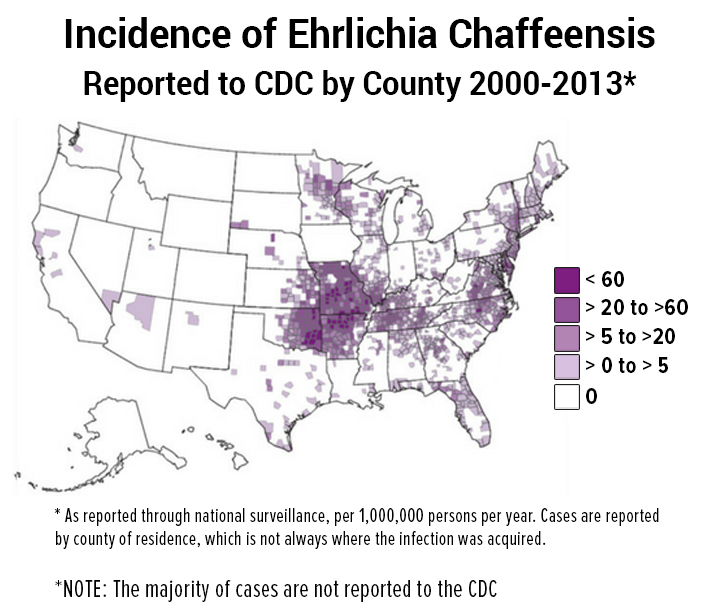
A ccording to the experts, ticks and the diseases they carry are expanding into new geographic areas. While the majority of Americans have heard of Lyme disease, fewer than 2% have any knowledge of another tick-borne disease called ehrlichiosis. 1,2
As a matter of fact, my own child was CDC-positive for an ehrlichial infection (amongst other things), and when I took her to the Emergency Room for an irregular heartbeat that developed during treatment, the ER doctor told me he had never heard of “Ehrlichia chaffeensis.” True story!
Warning!
In May 2017, an article in the CDC’s Emerging Infectious Diseases Journal warns that ehrlichiosis infections are being “grossly underreported” in the U.S., with as many as 97-99% of infections going unrecognized. They are projecting that the actual number of annual cases could go as high as 50% the number of Lyme disease cases—which would mean we may already have over 150,000 cases of ehrlichiosis annually. 3
There are several factors causing the underreporting:
- Lack of public education/knowledge—doctors aren’t testing for or diagnosing ehrlichiosis.
- Some cases are mild enough that patients do not seek medical care or a diagnosis.
- Insensitive or inaccurate testing methods may result in false-negative diagnoses.
- Reporting is voluntary and the criteria are restrictive.
Ehrlichosis
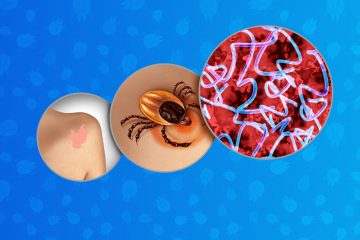
Ehrlichiosis is the name for several tick-borne diseases that are caused by a group of bacteria known as Ehrlichia. Ehrlichia belong to a larger order of bacterium known as Rickettsiales. 4 (See my previous post on the spotted fever group of Rickettsiae.)
Rickettsiae and Ehrlichia belong to a broad group of bacteria that can be spread by a tick bite. These infections can be transmitted alone or at the same time as Lyme disease and are commonly known as co-infections. (I talk more about co-infections here.)
The Ehrlichia (E) group includes: 5, 6, 7, 8
- chaffeensis: the cause of human monocytic ehrlichiosis (HME),
- ewingii, and
- muris-like (EML).
Symptoms
While some cases of ehrlichiosis are mild, the disease can be severe or fatal if not treated correctly, even in previously healthy people.
Severe symptoms of ehrlichiosis may include difficulty breathing, respiratory failure, bleeding disorders, and kidney or heart failure.
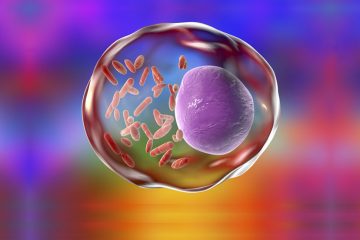
 Because Ehrlichia infect white blood cells (the cells that fight infection) and mitochondria (the powerhouse of the human cell), the consequences of untreated infection may have long-lasting effects.9 I often wonder if undiagnosed Ehrlichiosis isn’t responsible for some portion of the millions of people with the mysterious illness known as myalgic encephalomyelitis, or “chronic fatigue syndrome.”
Because Ehrlichia infect white blood cells (the cells that fight infection) and mitochondria (the powerhouse of the human cell), the consequences of untreated infection may have long-lasting effects.9 I often wonder if undiagnosed Ehrlichiosis isn’t responsible for some portion of the millions of people with the mysterious illness known as myalgic encephalomyelitis, or “chronic fatigue syndrome.”
Other symptoms of ehrlichiosis can include:
- Fever/chills and headache (majority of cases),
- Fatigue/malaise (over two-thirds of cases),
- Muscle/joint pain (25%–50%),
- Nausea, vomiting, and/or diarrhea (25% – 50%),
- Cough (25%–50%),
- Confusion or brain fog (50% of children; less common in adults),
- Lymphadenopathy (47%–56% of children; less common in adults),
- Red eyes (occasionally), and
- Rash (approximately 60% of children and 30% of adults).
Diagnosis and Treatment
Like other tick-borne diseases, diagnostic blood tests will frequently be false-negative during the first weeks of illness. And like other tick-borne diseases, treatment is most effective if started early. For this reason, healthcare providers must use their best clinical judgment and treat patients based upon early symptoms alone.
According to the CDC website:
The diagnosis of ehrlichiosis must be made based on clinical signs and symptoms, and can later be confirmed using specialized confirmatory laboratory tests. Treatment should never be delayed pending the receipt of laboratory test results, or be withheld on the basis of an initial negative laboratory result.
The CDC goes on to say:
Doxycycline is the first line treatment for adults and children of all ages and should be initiated immediately whenever ehrlichiosis is suspected. 10
Patients who are treated early may recover quickly on outpatient medication, while those who experience a more severe illness may require intravenous antibiotics, prolonged hospitalization, or intensive care.
Transmission
 The lone star tick (Amblyomma americanum) is the primary vector of E. chaffeensis (HME) and E. ewingii, with rates of infection ranging from 0 to 27 percent. In the past decade, the lone star tick has expanded into geographic areas where it did not previously occur. This is particularly concerning because the lone star tick is an aggressive biter.
The lone star tick (Amblyomma americanum) is the primary vector of E. chaffeensis (HME) and E. ewingii, with rates of infection ranging from 0 to 27 percent. In the past decade, the lone star tick has expanded into geographic areas where it did not previously occur. This is particularly concerning because the lone star tick is an aggressive biter.
While there is some geographic overlap, in general these ticks are found in the following areas:
- Lone star tick: east of the Rockies,
- Gulf Coast tick (Gulf and Southern states),
- American dog tick (east of the Mississippi),
- black-legged or “deer” tick (east of the Rockies), and
- western black-legged tick (west of the Rockies).

























If a person had bellspulsy long before the tick bite but suffered trigyminal neuralgia after the tick bite is this also one of the symptoms? It was on the same side of the face.
We suggest you consult with a Lyme-literate practitioner. Here is a link to our physician directory: https://www.lymedisease.org/find-lyme-literate-doctors/