Symptom Patterns in Six Lyme-Related Infections In "New Paradigms in Lyme Disease Treatment" 10 Top Doctors Reveal Healing Strategies
W hen mainstream medicine talks about Lyme disease, it’s usually couched in simple terms: A tick infected with one organism bites a person, causing a few specific symptoms. Treatment is a short course of doxycycline—and then you are good to go. Next!
Unfortunately, that’s not the experience of many people with Lyme disease. Instead of being infected with one errant pathogen, they may have several illnesses at once, causing a weird complex of symptoms that are difficult to sort out. Instead of needing just a short course of one specific drug—well, things are more complicated than that.
Author: Connie Strasheim
In the book New Paradigms in Lyme Disease Treatment, author Connie Strasheim interviews 10 doctors about their approach to treating Lyme-related illnesses.
In the following excerpt, Dr.Wayne Anderson
discusses six of the most common Lyme-related infections.
These symptom patterns should only be used as a guideline for diagnosis since no two people are exactly the same, and symptoms will vary from person to person. Neurotoxins from these infections all cause inflammation in the brain and nervous system and cause similar symptoms and compromise the body’s function in a similar way. Yet, each microbe often will manifest its own unique traits or personality.
Understanding the different symptom patterns that the microbes cause is especially important since lab tests for Lyme disease aren’t adequate (although they have improved greatly in recent years). Diagnosis also can be complicated by the fact that people’s immune systems respond differently to infection, according to their life stressors and metabolic strengths and weaknesses. Doctors should look for patterns in their patients and always appreciate that treating people with Lyme disease is about shades of gray, because the infections create symptom pictures that are never black and white.
Babesia or Babesia-Like Organism (BABLO) Symptom Patterns
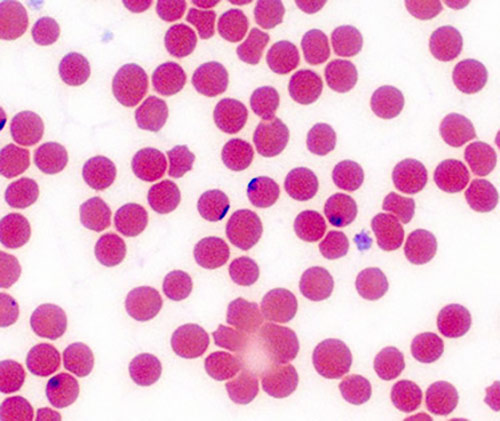 Babesia, or Babesia-like organisms (BABLO) primarily affect the brain and autonomic nervous system. The first words that a patient with active Babesia-like organisms in his body might say are that he can’t focus or think. His cognitive function is significantly compromised, and his mood is almost always affected. Both depression and anxiety are very common. A person with Babesia has a lot of emotional upheaval; fear is a dominant symptom.
Babesia, or Babesia-like organisms (BABLO) primarily affect the brain and autonomic nervous system. The first words that a patient with active Babesia-like organisms in his body might say are that he can’t focus or think. His cognitive function is significantly compromised, and his mood is almost always affected. Both depression and anxiety are very common. A person with Babesia has a lot of emotional upheaval; fear is a dominant symptom.
Babesia also can affect the autonomic nervous system, which is responsible for much of the “automatic” functions of the body, such as heartbeat, breathing, etc. This means that the communication between the brain and body is affected, so any physical symptoms that patients have from Babesia can be related more to autonomic nervous system dysfunction rather than the organisms themselves. For instance, Babesia can cause postural orthostatic tachycardia syndrome (POTS); a racing heart at rest and/or an irregular heartbeat and heavy pounding heart at night, but the problem isn’t in the heart. The problem is that the autonomic nervous system isn’t functioning properly.
Shortness of breath is also common, because people with Babesia don’t regulate their oxygen-saturation flow properly due to problems in the autonomic nervous system (ANS). Such people feel a sense of “air hunger” because the ANS isn’t dilating their bronchial tubes or opening their diaphragm properly, because these parts of their body are not getting the signal to do so from the command center in brain.
Additional symptoms of Babesia include lots of drenching sweats and chills. Babesia is a relative of the malarial organism and is part protozoan and part bacteria. So as with malaria, people can get terrible chills and lots of sweats and basically feel like they are going crazy. People with Babesia are often quite chilled and can’t get warm and will have to take a hot shower or jump in a bathtub to warm up. The temperature de-regulation is again related to a dysfunctional autonomic nervous system. So, people either can’t get warm, or they get too hot. They turn down the thermostat at night because they are too hot, but then they get too cold while in bed and so turn it back up by a degree. They freeze when going to bed and throw the covers on; then, in the middle of the night, they get boiling hot and throw the covers off and drench their bedclothes in sweat.
Insomnia is common as Babesia affects the sleep center in the brain. Other symptoms include blurred vision, bowel-motility issues and bladder difficulties. People with Babesia will either have trouble starting their urinary stream or will go through episodes of incontinence. They may also have problems with bowel motility; usually constipation, but can also sometimes have diarrhea due to autonomic nervous system de-regulation. A dominant Babesia infection also can affect certain areas of the wrists, hands, ankles and feet. These areas can be painful, numb or experience temperature extremes.
Babesia does not generally cause pain in the body, so if a person has pain, then it’s usually due to another problem. The picture is always complicated though because people with Babesia who have a compromised detoxification system will have pain in their body as a result of poor waste removal. But, the pain is not from the infection itself.
These are what I call clearly identifiable Babesia symptoms in those patients who have an immune system that is not terribly depleted or who don’t have a compromised detoxification system or other conditions or infections that are currently active and which could complicate the symptom picture. The same holds true for the symptom patterns of all of the other infections described here.
Bartonella or Bartonella-Like Organism (BLO) Symptom Patterns
 Many people have Bartonella or Bartonella-like (BLO) infections in their bodies. They are perhaps the most abundant infections in people because many veterinarians say that 80 percent of all house cats and nearly 100 percent of all hunting cats carry Bartonella microbes. Fleas bite cats and infect them with the Bartonella-like organisms, which are then transmitted to humans when they get bitten by the flea. Bartonella and BLO infections are therefore probably the most common of the vector-borne Lyme disease co-infections.
Many people have Bartonella or Bartonella-like (BLO) infections in their bodies. They are perhaps the most abundant infections in people because many veterinarians say that 80 percent of all house cats and nearly 100 percent of all hunting cats carry Bartonella microbes. Fleas bite cats and infect them with the Bartonella-like organisms, which are then transmitted to humans when they get bitten by the flea. Bartonella and BLO infections are therefore probably the most common of the vector-borne Lyme disease co-infections.
People who have active Bartonella symptoms have much more pain than people who are manifesting predominantly Babesia-related symptoms. The first thing out of their mouths is usually, “You have to help me with my pain.” They have pain in their joints and the connective tissue around their joints. This joint pain will migrate to other areas of the body. So for instance, patients with active Bartonella might have knee pain, but just when they are about to go to the doctor for the pain, the pain will migrate to the left elbow. The hallmark symptom of Bartonella is sensitivity and tenderness on the bottom of the feet, especially the soles.
Generalized pain in the body, or pain that is sharp and severe, is often related to Bartonella. Bartonella can also cause headaches and ice pick-like pain. Both Babesia and Bartonella cause headaches, but Bartonella headaches are worse. A Babesia headache produces more weird sensations in the head and pressure in the head. People with active Babesia infections will say, “I don’t know if I’d really call what I have a headache. It’s more like a pressure in the head.” Babesia can cause migraines as can Bartonella, but Babesia migraines are generally less severe. Bartonella prefers the occipital areas of the head; the back of the head and neck are generally painful. So pain is a dominant characteristic of Bartonella.
 All of these slow-growing intracellular infections affect the brain but create different symptom patterns, according to which infection is dominant or most active. I see more depression in people with active Babesia but less variability of mood, whereas people with active Bartonella may be irritable and anxious but then “flip over” into depression. Many people with Bartonella infections are misdiagnosed as having bi-polar disorder due to their fluctuating moods; they can easily go from being angry and irritable to being depressed.
All of these slow-growing intracellular infections affect the brain but create different symptom patterns, according to which infection is dominant or most active. I see more depression in people with active Babesia but less variability of mood, whereas people with active Bartonella may be irritable and anxious but then “flip over” into depression. Many people with Bartonella infections are misdiagnosed as having bi-polar disorder due to their fluctuating moods; they can easily go from being angry and irritable to being depressed.
Bartonella-like organisms can also stay on the surface of the organs and tissues and cause a wide array of symptoms. One such symptom is gastritis. In fact, most cases of gastritis that aren’t caused by Helicobacter pylori infections are often caused by Bartonella, which is the second-most common cause of this condition. It can irritate the stomach so that people lose their appetite and/or get heartburn.
Many people with Bartonella infections are misdiagnosed as having bi-polar disorder due to their fluctuating moods; they can easily go from being angry and irritable to being depressed.
Bartonella can cause a low-level, relapsing sore throat. People with active infections will periodically awaken with sore throats and wonder if they are coming down with a cold, but then the sore throat will go away.
Bartonella irritates the bladder and can cause frequent urination, interstitial cystitis, or other chronic inflammatory conditions of the urinary system.
Bartonella can also cause fevers, but for patients to be able to run a fever, they need to have a relatively functional immune system, so not everyone who has a Bartonella infection will get a fever. Yet people will often feel hot, as if they have a fever, but their body temperature may be below normal.
Bartonella can affect the eyes and cause conjunctivitis, or inflammation of the outermost layer of the eye, which results in irritated, dry red eyes, as well as other eye problems.
Bartonella cause more skin-related problems than the other infections. Red bands or stretch marks on the skin called striae are common, as are acne and other skin problems.
Bartonella lives in the liver and spleen where it inflames these organs and compromises their functioning. When the liver and spleen are inflamed, the filtering capacity of the blood is affected, resulting in thick blood. People with Bartonella may have slightly elevated liver enzymes on lab tests. For instance, the alanine aminotransferase (ALT) test score may be just outside of the normal range and high only intermittently. The inflammation that Bartonella causes in the liver and spleen can compromise the body’s detoxification system in a major way, though. When the spleen is compromised, the lymph glands may also become swollen, which then causes the lymph flow to become thick, sludgy and slow.
Borrelia Symptom Patterns
 Borrelia symptom patterns are a bit harder to define because this organism isn’t as aggressive as the others. The distinguishing symptom that it causes is fatigue; people who have active Borrelia symptoms tend to have more fatigue than those whose predominant symptoms are due to Bartonella or Babesia. People with active Babesia and Bartonella are much more restless than those with active Borrelia infections. All of the infections cause exhaustion; that is ubiquitous within the entire family of neurotoxin infections, but Babesia and Bartonella cause more restlessness, whereas people who are primarily manifesting Borrelia symptoms are often more tired. Feeling “wired and tired” is common with all the neurotoxin diseases, so I am really just focusing on the shades of gray here.
Borrelia symptom patterns are a bit harder to define because this organism isn’t as aggressive as the others. The distinguishing symptom that it causes is fatigue; people who have active Borrelia symptoms tend to have more fatigue than those whose predominant symptoms are due to Bartonella or Babesia. People with active Babesia and Bartonella are much more restless than those with active Borrelia infections. All of the infections cause exhaustion; that is ubiquitous within the entire family of neurotoxin infections, but Babesia and Bartonella cause more restlessness, whereas people who are primarily manifesting Borrelia symptoms are often more tired. Feeling “wired and tired” is common with all the neurotoxin diseases, so I am really just focusing on the shades of gray here.
Borrelia causes pain, but the pain is much more diffuse and spread throughout the body. It also can be muscle-related and fibromyalgia-like, rather than primarily in the joints, as with Bartonella. However, doctors and patients need to keep an open mind when it comes to diagnosis and not over-generalize about symptom patterns. For instance, there is a subset of Borrelia patients who have arthritic-like symptoms and lots of inflammation in their joints, although I see this maybe less than 10 percent of the time.
The symptoms of Borrelia can be a mixture of a little of what’s found in all of the other Lyme-related infections.
Borrelia affects the nervous system, but it’s a bit more “ghost-like” in the symptoms that it causes, so it’s not as defined or specific. If patients have been adequately treated for Babesia and Bartonella infections and have only 20 percent of their symptoms remaining, such as a bit of fatigue, achiness and brain fog, I might suspect that they still have some Borrelia microbes that need to be addressed.
Lyme microbes are smart and are looking for hiding places in the body; they want to be invisible and disguise themselves from the immune system. This means that they don’t stay in the blood for long and quickly go to areas of poor circulation, to avoid being attacked by the immune system. Their goal is to lull the intracellular environment into complacency. For instance, Borrelia is able to change its form and alternate between the spirochete, cell-wall deficient and cyst forms as a way of confusing and hiding from the immune system.
Editor’s note: Any medical information included is based on a personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.