The Agony of Mast Cell Activation Syndrome Mother recounts daughter's precipitous health decline from tick-borne illness and severe allergies to chemicals and food
I n the winter of 2016, my 17-year-old daughter was dying. She had severe allergic reactions every day, was in constant pain, and was losing weight at a rate that was not sustainable to life. She had reached the end of her rope, and I was completely out of ideas on where to turn for help.
 Eighteen months earlier, after a long illness and finally completing treatment for Ehrlichia chaffeensis, Bartonella and Lyme disease, she had been doing great. Unfortunately, she soon caught the flu and then everything went south. Over the next year, one setback after another landed her in the hospital every other month with atrial-fibrillation (irregular heartbeat) and/or near-anaphylaxis (acute allergic reactions). Each trip to the doctor took one more piece of hope away from us, since no one could pinpoint the cause of her rapid decline.
Eighteen months earlier, after a long illness and finally completing treatment for Ehrlichia chaffeensis, Bartonella and Lyme disease, she had been doing great. Unfortunately, she soon caught the flu and then everything went south. Over the next year, one setback after another landed her in the hospital every other month with atrial-fibrillation (irregular heartbeat) and/or near-anaphylaxis (acute allergic reactions). Each trip to the doctor took one more piece of hope away from us, since no one could pinpoint the cause of her rapid decline.
Over time, my daughter developed allergies to soaps, perfumes, juices, fruits, vegetables, and lunch meats. Eventually, she was down to only three foods that didn’t make her lips swell, mouth break out in blisters and throat tighten–chicken sautéed in our home-grown olive oil and brown rice noodles.
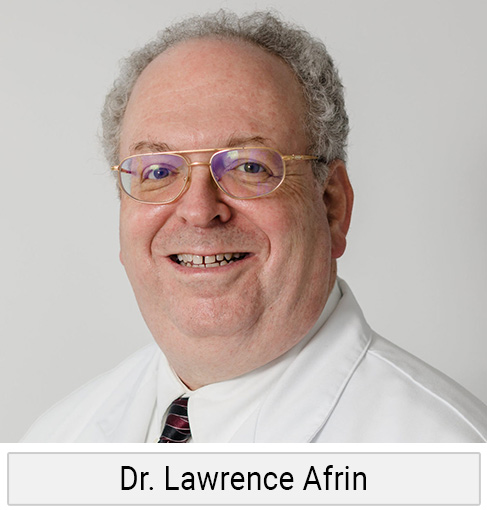 Not knowing what to do, I reached out in desperation to the “LymeParents” Yahoo group. Another mother recognized the symptoms I was describing as mast cell activation syndrome (MCAS) and connected me with Dr. Lawrence Afrin at the University of Minnesota. Dr. Afrin consulted on my daughter’s case, then referred us to Dr. Mark Renneker, a mast cell specialist at the University of California, San Francisco. Soon, she received a diagnosis of MCAS, and with it a path to healing.
Not knowing what to do, I reached out in desperation to the “LymeParents” Yahoo group. Another mother recognized the symptoms I was describing as mast cell activation syndrome (MCAS) and connected me with Dr. Lawrence Afrin at the University of Minnesota. Dr. Afrin consulted on my daughter’s case, then referred us to Dr. Mark Renneker, a mast cell specialist at the University of California, San Francisco. Soon, she received a diagnosis of MCAS, and with it a path to healing.
Coincidentally, one month after my daughter’s diagnosis, I attended Dr. T.C. Theoharides’ lecture on mast cell activation at ILADS in Philadelphia. In his words:
Mast cells are the “universal alarm cell” that starts the inflammatory cascade. They can be triggered by infection, allergens, environmental factors like pollution, or even emotional stress. Once that happens, mast cells set into motion a series of inflammatory reactions, including the activation of immune cells and the release of tumor necrosis factor-alpha (TNF-a), a pro inflammatory protein or cytokine.
If you or a loved one are in a similar situation, here’s what you need to know.
MCAS Diagnosis
MCAS is a clinical diagnosis based upon signs, symptoms, and response to treatment. There are several tests available to confirm the diagnosis, but negative tests do not rule out MCAS.
Mast Cell Activation Diseases
 Mast cells are a normal part of our immune system. They are located in every tissue of the body, but in higher concentration in areas of the body that come into contact with the outside world (eg. skin, sinuses, throat, lungs, gastrointestinal tract, etc.) When mast cells detect stress, injury, toxins or infection, they release specific chemicals which trigger an immune response. Think of them as sentries or guards.
Mast cells are a normal part of our immune system. They are located in every tissue of the body, but in higher concentration in areas of the body that come into contact with the outside world (eg. skin, sinuses, throat, lungs, gastrointestinal tract, etc.) When mast cells detect stress, injury, toxins or infection, they release specific chemicals which trigger an immune response. Think of them as sentries or guards.
When mast cells perform properly, they are our friends. When mast cells are agitated or over-reactive, the immune system goes haywire and starts to attack the body, triggering auto-inflammatory processes or some types of autoimmune illnesses.
- Mastocytosis — the abnormal accumulation of mast cells in one or more organ systems (cardiovascular, central nervous, digestive, endocrine, genitourinary, lymphatic, muscular, peripheral nervous, respiratory) which is diagnosed by a bone marrow biopsy or a C-Kit genetic mutation.
- Mast Cell Activation Syndrome — the inappropriate release of mast cell mediators including: histamine, interleukins, prostaglandins, cytokines, chemokines, and heparin.
As far back as 1999, researchers were able to demonstrate how Borrelia burgdorferi induces mast cell activation, contributing to greater illness in Lyme disease. Somehow, I feel this fact has remained under-appreciated until just recently.
PTSD of the Immune System
 When I describe my daughter’s condition to non-medical folks, I say it’s like her immune system has post-traumatic stress disorder (PTSD). After going a year with multiple untreated infections, her immune system was depleted, and the combination of antibiotics she needed to fight her infections added additional stress. As she completed antibiotic treatment for her infections, we added supplements to boost her immune system and promote healing. Or so we thought.
When I describe my daughter’s condition to non-medical folks, I say it’s like her immune system has post-traumatic stress disorder (PTSD). After going a year with multiple untreated infections, her immune system was depleted, and the combination of antibiotics she needed to fight her infections added additional stress. As she completed antibiotic treatment for her infections, we added supplements to boost her immune system and promote healing. Or so we thought.
Unbeknownst to her doctors and me, one of her prescription medications (ketotifen) contained lactose, to which she is intolerant. In addition, she had developed an allergy to microcrystalline cellulose (MCC), one of the most common fillers in prescription medications, vitamins, and supplements. Eliminating these two allergens was a major turning point in her healing.
Accepting that you have a problem
This is a tough one. It reminds me of my daughter’s childhood friend, who was diagnosed with diabetes in second grade. After years of failing oral medications, he eventually received an insulin pump that inserts directly into his abdomen. It completely changed the type of sports he could play and the way he had to live his life. But within a year, he had adjusted and could do nearly everything other kids his age did, as long as he adhered to a routine.
My daughter had to come to grips with the fact that she may never be able to roll in the grass or eat many of her favorite foods again. She also had to accept that she lost five years of her life and a lot of childhood dreams. Not only that, but fighting our way through the medical system to a diagnosis and treatment left a lot of emotional scars and a type of trauma caused by medical treatment (iatrogenic)– very similar to post-traumatic stress disorder (PTSD). This is where I truly believe a compassionate therapist is needed.
So, to me, healing from MCAS not only requires lowering histamine levels and retraining your immune system, but also retraining your mind, creating a safe environment within your restrictions, and designing a lifestyle that continues to bring you joy.
Our Five Steps to Healing
Reduce or eliminate mast cell triggers (common triggers)

- Infection (bacteria, fungi, parasite, virus)
- Insect bites (spiders, ticks, fleas, mosquitos, bed bugs)
- Stress (heat/cold, weather changes, fatigue, emotional stimuli)
- Foods (dairy, high histamine foods, fermented or aged foods, wheat, shellfish, sugar, certain preservatives)
- Drugs (alcohol, opioids, aspirin, NSAIDS, excipients, other medications)
- Dyes (food coloring, radiographic dyes, pigments in makeup)
- Environmental toxins (pollen, dust, mold, animal dander, heavy metals, pesticides)
- Noxious odors (perfumes, smoke, exhaust fumes, smog)
Assemble the “A TEAM” (example)
- Physician knowledgeable about Lyme and other tick-borne diseases (treat infections)
- Physician knowledgeable about mast cell activation syndrome (lower histamine, stabilize mast cells)
- Psychotherapist (emotional support, lower stress)
- Physical therapist (modalities for pain, cranial-sacral therapy, lymphatic drainage, home care instructions)
- Doctor of Osteopathy (functional medicine, supportive hands-on therapy)
Working with your team, find the right combination of medications/supplements
 Many people with mast cell issues will improve by taking antihistamines. Antihistamines are medications that block or inhibit the histamine receptors on mast cells and other cells found throughout the body.
Many people with mast cell issues will improve by taking antihistamines. Antihistamines are medications that block or inhibit the histamine receptors on mast cells and other cells found throughout the body.
Histamine is a unique chemical produced primarily by mast cells that causes inflammatory reactions and the itching feeling most of us are familiar with. Histamine also signals the immune system, regulates the digestive system, and acts as a neurotransmitter in the brain, spinal cord and uterus.
Caution: Most MCAS patients are hypersensitive. My advice when trying anything new is to go low and slow. Micro test the first dose. If no reaction, wait a day or two and try again. If you find something that works, don’t assume more is better. Try not to add more than one new medication in a four-day period, as this makes it too difficult to detect which one is helping or potentially hurting the condition.
We ran a complete vitamin and mineral panel to pinpoint nutrient deficiencies. Then, we designed a custom nutrition plan that was specific to her needs. Basic diet: Clean, fresh (nothing cured, processed, or fermented), organic, gluten-free, dairy-free, dye-free, sugar-free, low-histamine, low-citrus, low-oxalate, low-nightshade, also consider elements of a low FODMAP diet.
Customize Nutrition
Patients with certain genetic defects are more prone to MCAD. Looking into your genetics can help determine your predisposition to MCAD and/or histamine intolerance and help you design a customized nutrition plan.

- KIT-D816V — KIT is a master regulator protein found on and in mast cells. A KIT mutation typically results in the mast cell being constantly activated. About 90% of patients with mastocytosis have a KIT-D816V mutation (there is a PCR test for this mutation).
- MTHFR — The body makes several enzymes called MTHFR that are critical for the production of folate and many cellular functions. Patients with MTHFR defects may have an inability to clear histamine leading to MCAS and histamine intolerance.
- HNMT — In the central nervous system, histamine is broken down by histamine methyltransferase (HNMT). Patients with a lot of HNMT defects will have trouble clearing histamine from the brain and nerves. Moodiness, sleep disturbance and frequent rashes or hives can be a sign of this.
- ABPI — In the digestive tract, histamine is broken down by diamine oxidase enzymes (DAO). Defects in ABPI lead to lower levels of DAO and higher levels of histamine.
- HLA — Variations in the HLA gene can increase the chances of gluten intolerance.
- VDR — VDR defects may lead to lower levels of Vitamin D, which is critical to immune health.
- MAT — MAT gene is involved in the conversion of the amino acid methionine into SAMe. SAMe has 100s of critical functions throughout the body. If vitamin B12 makes you feel sick, you may have a lot of MAT defects. Your doctor can order blood work to check methionine and SAMe levels.
We ran a complete vitamin and mineral panel to pinpoint nutrient deficiencies. Then, we designed a custom nutrition plan that was specific to her needs.
Basic diet — Clean, fresh (nothing cured, processed or fermented), organic, gluten-free, dairy-free, dye-free, sugar-free, low-histamine, low-citrus, low-oxalate, and low-nightshade. You might also consider elements of a low FODMAP diet (a specialized elimination plan to help you identify which foods are troublesome for you).
Stick to a Routine
- Avoid stressful situations
- Maintain the same sleep schedule
- Maintain the same eating schedule
- Maintain the same basic level of activity from day to day
- Pace yourself and avoid overexertion.
Putting it all together
These steps may seem daunting. But when you are in a crisis like my daughter was, you are willing to go to extremes to get your life back.
References:
- Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3069946/.
- Borrelia burgdorferi Spirochetes Induce Mast Cell Activation and Cytokine Release https://www.ncbi.nlm.nih.gov/pmc/articles/PMC96436/.
- Recent Publications and Presentations by Theoharis C. Theoharides, Ph.D., M.D. http://mastcellmaster.com/publications.php.
Editor’s note: Any medical information included is based on a personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.