TOUCHED BY LYME: Real-world patient data can help find a cure
I wrote the following article, which appeared in the July 2020 issue of the “Townsend Letter: The Examiner of Alternative Medicine.”
MyLymeData is a patient registry and research platform launched by LymeDisease.org in 2015. Using big data research tools, it allows patients to privately pool information about their Lyme disease experiences. They answer questions such as how long they have been sick, what treatments they have tried, and what has and has not worked for them.
When Lyme disease is diagnosed and treated early, most patients are restored to health. However, even in patients diagnosed and treated in the acute phase, many remain ill after treatment. In addition, delays in diagnosis often makes treatment more difficult. Lorraine Johnson, CEO of LymeDisease.org and Principal Investigator of MyLymeData, says the organization started the project because of staggering unmet needs of the community for prompt diagnosis and effective treatment.
“Huge numbers of people with Lyme disease do not get diagnosed and treated in the early phase of the illness, when treatment is most successful,” Johnson says. Unfortunately, this allows the pathogen to get deeply entrenched in the body, making it more difficult to eradicate. Protocols developed for the acute illness do not appear to be effective for long-term Lyme disease.
Unfortunately, there has been little research into how to help people who suffer persistent Lyme symptoms. “Lyme disease is extremely research-disadvantaged,” says Johnson. The National Institutes of Health (NIH) has funded only three treatment trials for Lyme disease, with small samples. For instance, the treatment group in the largest NIH trial enrolled only 64 patients. “The problem with small trials is that they don’t give you much information,” says Johnson. Furthermore, recruitment for those trials took place 20 years ago, with nothing in the pipeline since then.
More than 3 million data points
In contrast, more than 12,000 patients have enrolled in MyLymeData, providing over three million data points on Lyme disease demographics, tick bites, diagnosis, symptoms, lab tests, co-infections, treatment and quality of life. The results have been eye-opening.
- 70% of those in the registry were not diagnosed until six months or more following the onset of their symptoms. Most patients take three or more years to diagnosis and see five or more clinicians. Studies show that patients diagnosed late are less responsive to short-term antibiotic treatment.
- Fewer than 12% of patients in the registry were diagnosed within the critical first month. Most patients who are diagnosed and treated early respond well to short term treatment protocols.
- 74% reported early symptoms of the disease, but only 34% recall having the distinctive erythema migrans rash (EM) commonly relied on by physicians for diagnosis. More common early symptoms were flu-like symptoms (64%) and severe headache or stiff neck (44%). Patients who do not have an EM rash are more likely to be misdiagnosed.
- 60% report that they have been diagnosed with an additional tick-borne infection, such as babesiosis or ehrlichiosis. The presence of co-infections may increase the likelihood of developing chronic Lyme disease.
- 72% of patients with chronic Lyme disease report that they were initially misdiagnosed with another condition. Patients misdiagnosed with another condition experience diagnostic delays and may be exposed to adverse effects from treatments for diseases that they do not have.
Peer-reviewed study published
In 2018, the first peer-reviewed study using information from MyLymeData was published in the medical journal Healthcare. Using patient-reported outcome data from over 3900 registry patients, it looked at how individual Lyme patients vary in their response to antibiotic treatment.
Using a widely validated global rating of change scale, the MyLymeData team identified subgroups of patients who responded differently to treatment. Fifty-two percent reported at least some improvement with antibiotic treatment—with 34% reporting substantial improvement with treatment. Thirty-seven percent had no treatment response at all and 12% were worse after treatment.
Why do patients respond so differently to treatment? Do some of them have co-infections, were there diagnostic delays, different treatments or treatment durations? So far, that is unknown, but examining real-world data from registry patients may provide the path to more individualized care. “Such subgroup analysis of large samples allows us to uncover critical information that otherwise may not be available,” says Johnson.
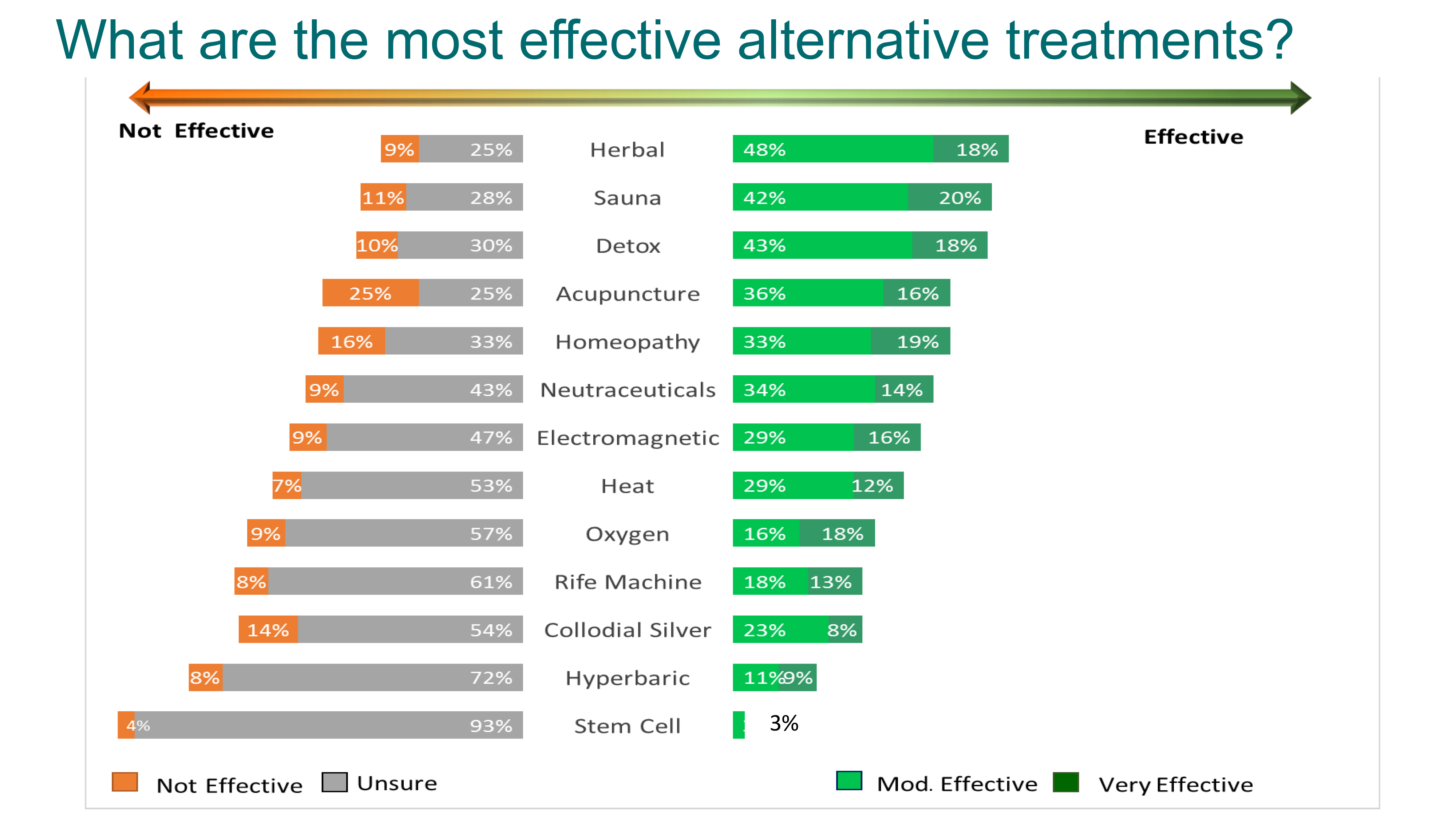
Alternative treatments
MyLymeData also asks questions about alternative treatments for Lyme disease. Patients who use alternative treatments either use them in conjunction with antibiotics (38%) or as a sole means of treatment (31%). The most popular alternative treatment included herbal protocols, sauna, chelation, and medical marijuana.
Important considerations for selecting any treatment modality include effectiveness and side effects. Herbal protocols, many of which have antimicrobial properties, are among the most popular. Sixty-eight percent of patients who used them reported that they were either moderately or very effective, with few side effects.
The MyLymeData team works with academic researchers at the University of California, Los Angeles and the University of Washington. The National Science Foundation has funded the UCLA researchers to explore big data analytics using information from MyLymeData. The registry also collaborates with the Lyme Disease Biobank, a Bay Area Lyme Foundation program. In addition, MyLymeData can assist with clinical trial recruitment, augment clinical trial research findings, and generate hypotheses for further clinical studies.
“We view the patient registry as a vital part of a research engine that can accelerate the pace and increase the depth and breadth of Lyme patient research,” says Johnson. “At the same time, we take patient privacy seriously.” Accordingly, LymeDisease.org vets researchers and restricts data use and re-use, to ensure that patient data is used solely for the benefit of Lyme disease patients. “Many big data projects sell data to third parties like pharma or insurers,” cautions Johnson. “We do not. We make sure that patient data is used for the benefit of patients—period.”
In 2019, LymeDisease.org published a 36-page full color chart book of highlights from MyLymeData. Click here to download a free PDF copy.
Patients interested in participating in the MyLymeData patient registry should visit www.mylymedata.org.
Click here to learn more about the Townsend Letter.
LymeDisease.org advocates nationally for quality accessible healthcare for patients with Lyme and other tick-borne diseases. We are committed to shaping healthcare policy through science-based advocacy.
Dorothy Leland is Vice-president and Director of Communications for LymeDisease.org. She can be contacted at dleland@lymedisease.org.
References
Johnson, Lorraine (2019): MyLymeData 2019 Chart Book. figshare. https://doi.org/10.6084/m9.figshare.8063039.v1
Johnson L, Shapiro M, Mankoff J. Removing the Mask of Average Treatment Effects in Chronic Lyme Disease Research Using Big Data and Subgroup Analysis. Healthcare (Basel). 2018 Oct 12;6(4).
https://res.mdpi.com/d_attachment/healthcare/healthcare-06-00124/article_deploy/healthcare-06-00124.pdf.




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page