Making Sense of Lyme Research – What Does the Science Say?
by Nicole Danielle Bell
When I finally realized that my husband’s early-onset Alzheimer’s was caused by Lyme disease and other co-infections, I tried to use my engineering background to make sense of it all.
I very quickly found myself lost. An excerpt from my memoir about our experience shows how confused I was as a newly minted caregiver.
January 2018 – Lost in the literature
(Excerpt from “What Lurks in the Woods: Struggle and Hope in the Midst of Chronic Illness”)
I poured every spare moment into research. Of course, I started where everyone starts: the Internet. I quickly realized what I already knew. The Internet was a dangerous place to get information. My searches left me more confused than when I started.
Half of the articles insisted that chronic Lyme didn’t exist. The Centers for Disease Control and Prevention, the CDC, claimed Lyme could be treated with two to four weeks of antibiotics. After that, anyone still sick didn’t have chronic Lyme; they had Post-Treatment Lyme Disease Syndrome or PTLDS. But the causes of PTLDS were unknown. It could be an autoimmune response triggered by the bacteria. It could be a persistent but difficult to detect infection. It could be other issues unrelated to Lyme. As I read their position over and over again, it didn’t make sense. One of their explanations for PTLDS was a “persistent but difficult to detect infection.” Um, okay. Why couldn’t that be Lyme?
The other half of the articles blamed Lyme for nearly every chronic disease on the planet: fibromyalgia, arthritis, chronic fatigue syndrome, multiple sclerosis, myocarditis, Parkinson’s, Alzheimer’s, scleroderma, depression, schizophrenia. The bacteria was invading our immune system and wreaking havoc. It infected joints, brain tissue, and cardiac tissue. It triggered autoimmune conditions, dementia, and mental illness. The disease was way under-reported and globally prevalent, not only in the American Northeast.
So, what to believe? Frustrated, I turned away from Internet articles and turned toward scientific articles on PubMed. The messages there were equally mixed. I scanned through titles and abstracts. For each article I found supporting chronic Lyme’s existence, I found another attempting to debunk it. Clearly, I needed to read the articles to form my opinion, so I dug in. I found observational studies with no controls, failed attempts to reproduce past results, citations to other papers that didn’t say what was claimed. The more I read, the more frustrated I became.
I had long been a steward of science. “In God we trust; all others must bring data.” The quote from W. Edwards Deming was frequently touted at the FDA and always made me smile. I agreed. Data was pure. Data had no agenda. Data was just data.
But my career taught me this wasn’t true. Data collected was only as good as the methods used. Science used mice and cell cultures that may not represent the complexity of a human. Researchers interpreted the data, and often their bias skewed the results. I’d seen engineers interpret the same results in opposite ways. Plus, people made mistakes.
I once struggled for over a month with an experiment, having no idea why the results didn’t match the theory. Then, I spent the day with my technician and realized that every time I instructed her to do a step for a minute and a half, she entered one minute and fifty seconds into the machine, completely trashing my analysis. Data wasn’t always pure. It could be flawed.
I saw this debate raging in the medical community, and I didn’t know whether to feel vindicated for finally finding my answers or crazy for believing in something so clearly outside mainstream medicine. Organizations like the CDC and the Infectious Disease Society of America should know what they are talking about, right?
On the other hand, mainstream thinking always evolves, even in science. If it didn’t, we would still think the world was flat or that lobotomies were the best way to treat mental illness. No one believed that the bacteria H. pylori caused stomach ulcers, so Dr. Barry Marshall infected himself to prove it. Nutritional guidelines in the 1980s told us a low-fat diet was best. Now, leading experts tout that a high-fat, ketogenic diet is better for overall health. I needed to navigate a complex infectious disease, and I couldn’t get a straight answer on eggs. Good for me? Bad for me? Different doctors, different answers. Argh! I was in the middle of a debate where my husband’s life hung in the balance. I had the desire to learn and the skills to understand, but I was more lost than ever.
October 2022 – A second chance to make sense of it all
My husband’s story didn’t end well. He lost his battle with tick-borne illness and passed away in January of 2022, a broken shell of the man he once was. Devastated, I turned my energy into sharing our story and driving change for future patients.
My networking efforts connected me with researchers striving to develop new diagnostics and therapies, philanthropists funding new approaches and studies, and advocates seeking to raise awareness and funds for this critical problem. One of those advocates was Bonnie Crater, a co-founder of the Center for Lyme Action.
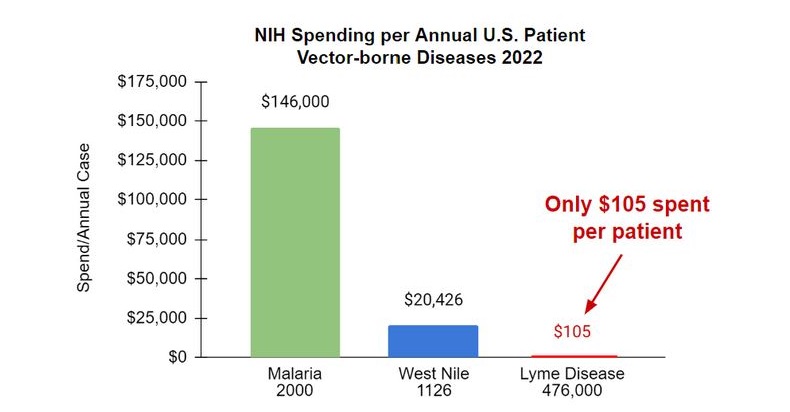
Bonnie explained that part of the reason the available Lyme literature and information was so confusing and incomplete was that federal research funding is insufficient. Lyme disease accounts for the vast majority of vector-borne illnesses in the United States; however, it is funded at a fraction of other diseases.
The CDC estimates that 476,000 Americans are diagnosed and treated for Lyme annually; however, funding at the National Institutes for Health (NIH) for Lyme Research was only $50M in 2022. This calculates to $105 per patient, representing 0.1% and 0.5% of the per-case funding for malaria and West Nile virus, respectively.
The Center for Lyme Action was established to change this funding scenario. For their 2023 efforts, they wanted a paper summarizing “The State of Lyme Disease Research in the United States.” This document would review the evidence and highlight government action and research funding opportunities. But the project needed a writer, and after reading my book, Bonnie was convinced that writer was me.
I was honored by Bonnie’s confidence, but I wasn’t so sure. It was a daunting project, and flashbacks to my previous attempt to dig into the research haunted me. But the more I thought about it, the more I realized I had to do it.
I had to do it for my husband, Russ, who had needed this summary in 2018 – or sooner. I had to do it for the millions of patients struggling with their chronic symptoms. And I had to do it for the millions of people who will become infected and fail to get a timely and accurate diagnosis.
Fortunately, the evidence has evolved since my time as a caregiver. Panels of experts weighed in as part of the Federal Tick-Borne Disease Working Group (TBDWG). The TBDWG was a six-year process, issuing reports in 2018, 2020, and 2022, reviewing the status of the research, and making recommendations for government action.
Per the recommendations of their 2018 report, the National Institutes of Health (NIH) convened a trans-NIH strategic planning team. In 2019, this team released a comprehensive Strategic Plan to improve tick-borne disease diagnosis, prevention, and treatment. I could leverage all of this work in the paper. Finally, Bonnie agreed to connect me to a network of leading Lyme researchers to guide and review the document.
July 2023 – The summary I wish I’d had and changing tides
The process of producing it was invaluable, not only because of what I learned but also because it demonstrated to me and hopefully others that the problems Lyme disease patients face ARE solvable. Research shows that Lyme IS linked to chronic conditions across multiple body systems. New diagnostics and treatments ARE promising, but more funding is needed to get them out of the research lab and into the clinic.
And the tide is turning in mainstream thinking. The Department of Health and Human Services (HHS) has begun using the term “infection-associated chronic illness,” and the National Academies of Sciences, Engineering, and Medicine recently held a workshop to discuss these conditions, including persistent Lyme disease.
And the tide is also turning on a disease near and dear to my heart, Alzheimer’s. New research reported at the Alzheimer’s Association International Conference in 2021 found associations between COVID-19 and persistent cognitive deficits, including the acceleration of Alzheimer’s disease pathology and symptoms.
These findings have rekindled scientific interest in the link between neurological infections and the progression of dementia, with the National Institute of Aging offering a virtual workshop on the Infectious Etiology of Alzheimer’s Disease in October of 2021.
In addition, last month, a consortium of scientists called for the establishment of a consensus protocol to explore the role of infections, such as Lyme disease, in patients with mild cognitive impairment and Alzheimer’s disease – a battle I fought with neurologists only a few years before.
The future – what you can do to drive change
“The State of Lyme Disease Research in the United States” aims to educate Congress on the breadth of the problem and how they can fix it. The NIH Strategic Plan released in 2019 was comprehensive, and that plan and the recommendations of the Tick-Borne Disease Working Group need to be funded and implemented.
So what can you do? You can sign onto the Center for Lyme Action mailing list at centerforlymeaction.org. Scroll to the bottom of the home page, and you’ll get a pop-up form for sign-up. Several times a year, you’ll get notifications of activities and actions you can take to grow federal funding for Lyme and tick-borne disease. By signing up, you will also be invited to participate in the annual “Lyme Fly-In,” an opportunity to speak directly with your Senator or Member of Congress’s office.
But I hope that “The State of Lyme Disease Research in the United States” goes beyond congressional action. If you are a patient or a caregiver, I hope it provides the scientific evidence you need to understand that you aren’t crazy, and it’s not in your head. I hope you give a copy of the paper to your doctor and it helps your doctor understand the realities of Lyme disease and the status of the research. And I hope it helps you or your loved one get a timely diagnosis and effective treatment.
Click here to read “The State of Lyme Disease Research in the United States.”
Nicole Bell is the author of What Lurks in the Woods: Struggle and Hope in the Midst of Chronic Illness.




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page