Why do some Lyme patients improve with treatment and others don’t?

Press release from LymeDisease.org, June 8, 2017:
A new study suggests that developing effective treatments for Lyme disease may depend on understanding which patients respond to different treatments.
Data collected from over 3,400 patients through LymeDisease.org‘s MyLymeData online patient registry suggest that big data analysis techniques can identify subgroups of patients that respond well to treatment.
Some chronic Lyme disease treatment studies done in the past have failed to identify treatment successes, but relied on samples of patients too small (37-129 patients) for subgroup analysis.
Finding effective treatments is critical. Over a third of those diagnosed and treated for Lyme disease develop persisting debilitating symptoms following short-term antibiotic therapy. According to the CDC, at least 380,000 people are diagnosed with Lyme disease in the U.S. every year.
(PRNewsfoto/LymeDisease.org)
At PharmaSUG’s recent Baltimore conference, biostatistician Mira Shapiro presented a paper examining how much patients’ condition changed following antibiotic treatment.
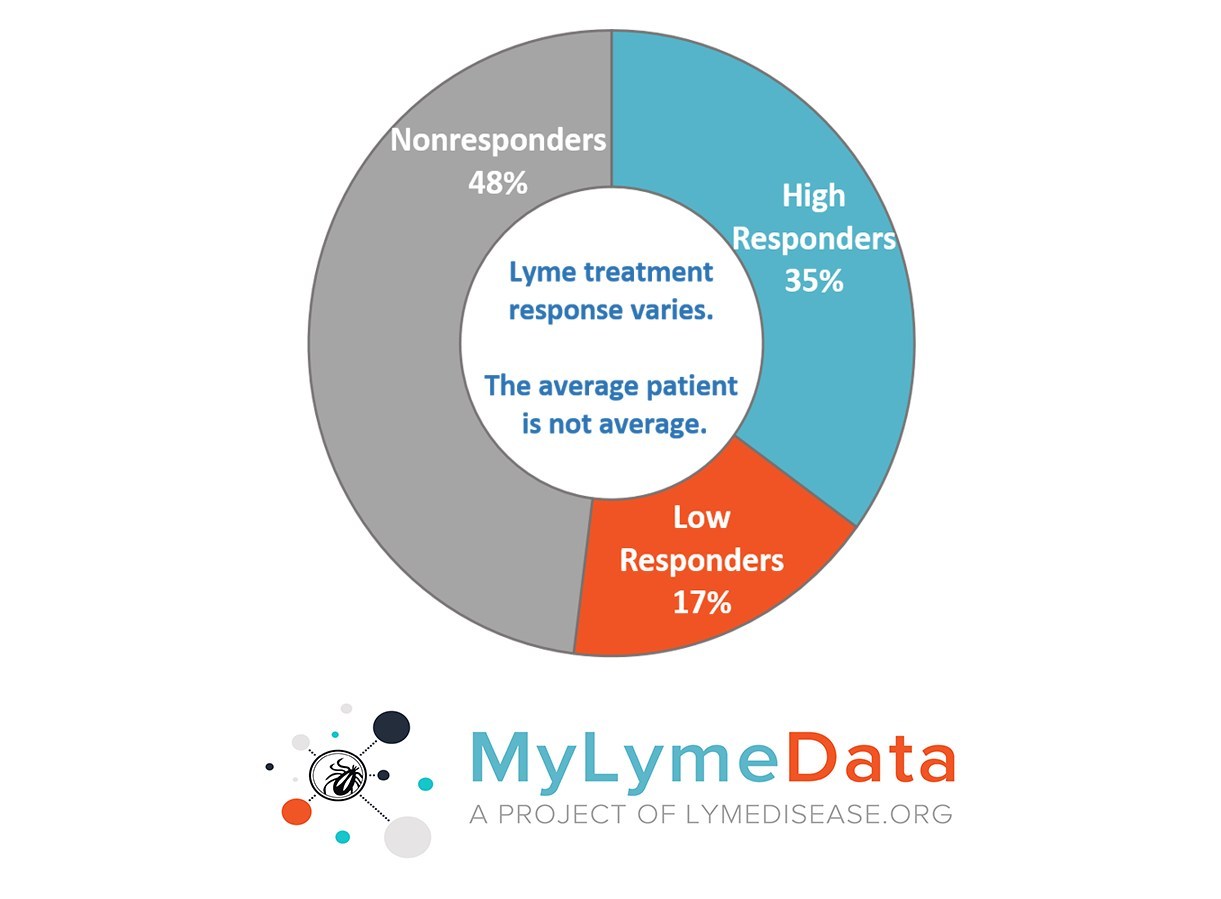
When treatment response was averaged over all patients in the sample, treatment effects were small. However, when patients were broken into three subgroups, it was clear that some patients reported a large treatment effect while others reported minimal or no treatment effect.
The survey used a global rate of change scale, typical of those used by clinicians in practice. Patients reported whether their condition was improved, unchanged, or worse on a 15-point Likert Scale, used in studies of other diseases. Response choices ranged from “a very great deal worse” to “a very great deal better,” with a midpoint of “unchanged” or “almost the same.”
Responses were grouped into three categories: High Responders (“moderately better” to “a very great deal better”), Low Responders (“hardly better at all” to “somewhat better”) and Nonresponders (“no change” to “a very great deal worse”).
Forty-eight percent of the patients in the study were characterized as Nonresponders. They reported that their condition had either gotten worse or had not changed following treatment. More than 50% of patients surveyed reported some degree of improvement. Thirty-five percent were High Responders, while Low Responders accounted for 17%.
Subgroup analyses involves splitting participant data into subgroups to permit comparison between the groups. Shapiro says that big data allows us to identify important subgroups that respond to treatment.
“Patients with chronic Lyme disease vary in their response to treatment,” she explains. “Averaging results across patients can mask important differences in treatment response.”
According to Lorraine Johnson, JD, MBA, Chief Executive Officer of LymeDisease.org and coauthor of the study, this type of analysis is the key to improving the lives of Lyme disease patients.
“Other diseases like tuberculosis categorize patients into groups based on how they respond to treatment. It’s time for Lyme disease research to enter the 21st Century,” she says.
Since its launch in November 2015, MyLymeData has enrolled over 8,000 patients in its registry. This study included registry data compiled from 3,400 patients who self-identified as “unwell” during Phase 1 of the project, which was completed in November 2016. Patients in this preliminary study reported living in the United States, being diagnosed with Lyme disease by a healthcare practitioner and receiving antibiotic treatment.
The newest phase of MyLymeData is open to both current and new enrollees who may register at LymeDisease.org. Patients currently participating in MyLymeData simply log into their accounts to complete the new survey sections.
Click here for more information about MyLymeData.
About LymeDisease.org
Since 1989, LymeDisease.org has advocated nationally for quality accessible healthcare for patients with Lyme and other tick-borne diseases. We are committed to shaping healthcare policy through advocacy, legal and ethical analysis, education, physician training, and medical research. Our mission is to prevent Lyme disease, prevent early Lyme disease from becoming chronic, and to obtain access to care for patients with chronic Lyme disease.




















I think you would have to know more about how the patients interpreted the question. Some may say no improvement because they have not been cured. Some may say no improvement because they still have untreated or undertreated coinfections, and still more possibilities.
This kind of research is dealing with a heterogeneous group, at various stages of the disease, so it will be by definition deliver less than pinpoint accuracy. It is a good start, but one should not conclude that a large number of people were not helped by treatment. This is a messy situation and the results will reflect it.
How much time after treatment began were they surveyed. In the short term many experienced herx effects and felt worse before beginning to improve.
I had trouble with the survey, because I did 3 years of treatment, had major 70% improvement, then relapsed in mid 2016 and am struggling heavily with this relapse still. On one hand, many symptoms disappeared (bladder, joint pain) but others have come back (Bab’s related POTS, insomnia, migraines, breathing and major fatigue) leading me back to a 30% improvement from the start of treatment. It’s a complicated issue and the survey (as much as I admire the work that went into it) is too narrow to describe treatment progress. I’m not really even sure if it’s possible to widen the scope of a QA, because of the complexity and range of the illness. I think maybe some Q&A that focuses on various times in treatment that things improved and for how long they improved then relapse and how long the relapse is. It’s such a complex disease unique to each person, I can’t imagine trying to create a survey to understand the disease/treatment in a general way. Though I understand that is not the intent. I truly applaud the survey efforts and will continue to use it through my own treatment.
I think that the most important variable is the amount of time the person has been infected before treatment is given. This is also an unknown since many persons are bitten and infected without their knowledge. (Remember that these ticks are frequently too small to see.) Another issue is the other vector-borne infections that are transmitted at the same time as Lyme. Still another is re-infection (or additional), and with what infections. Last, there are other factors that can cause a “normal” reaction to kill off an infection to be halted or dampened, such as a major trauma, physical and/or emotional.
I was diagnosed with Lyme by Western Blot, after being bedridden for about 1 1/2 years, in 1989. I was also in a automobile collision in July 1988 that caused major injuries to me.
I am awaiting serological and autoimmune blood results from Tropical and Infectious Diseases Hospital in London. January 2015 tick bite South Downs, England cellulitis diagnose after ignore my protestations that I saw the tick attached to left calf. Am retired SRN and am appalled at lack of knowledge by the Medical profession but am in disbelief regarding g listening and believing g the patient/client. After STEMI, NSTEMI, CVA, peripheral neuropathy and continuous low grade fever and horrendous head pain could stand it noore and took myself to said hospital A&E and asked a nuse for advice. Following conversation and subsequent action had an appointment a week later.
I have a “need to know” attitude. Years in my life ? At 77 it is life in my year, quality of which is questionable at the moment.. my natural optimism a no doubt annoying insistence keeps me going….
I responded exceptionally well upon very late treatment of lyme, but never got as well as I should have. I was near death by the time treatment began, and had it for several decades.
After 15 yrs of treatment, it seemed I was gradually going downhill after the initial huge improvement. I had numerous blood tests for several tick borne diseases over the years after treatment began, and nothing ever showed up.
Here’s the big changer in the game.. I got a PCR DNA test done as finally those were available.
Wow! Not only did the Lyme show for the first time ever, but also Babesia, Bartonella, and Erlichia!
We’re just going to be starting on Babesia protocol, and the others will follow. I don’t really have much in the way of true Lyme disease symptoms as I used to, but do have profound symptoms of the others. All this time I assumed it was still the Lyme.
I wonder if lots of other people are also simply undiagnosed with the complete array of diseases they have and are not being treated for those, rather than being “non or low responders.”
~ Ann microtyger ~
I was diagnosed in early fall of 2016. My Lyme was caught quickly as I went to the Dr. having flu like symptoms but very weak. I had a huge purple/red oval on my inner thigh and the Dr. immediately diagnosed me with Lyme and followed up with blood work. I was given 2 rounds of antibiotics and returned to good health. In late March of 2017 I started having problems with extremely cold hands and feet. I brushed it off for a couple of weeks and then returned to the Dr. We are still trying to figure out what the cause might be. I just saw a rheumatologist last week and they completed some blood work suspecting perhaps Reynalds. I keep asking if this could be a result of Lyme and nobody seems to know. Anyone have any information out there as to whether we should suspect this might be so, or others who have experienced this. Vascular scans were negative.
I am being treated for Lyme, Babesia and Bartonella. Its been about 6 months now and responding well to treatment. One of my complaints or symptoms for the past 3 years has been cold hands and feet. To the point of tingling and itchy feeling- really annoying. Soaking my feet in hands in hot water would help. It seems to be getting better so i do relate to the tick borne diseases i have.
Barbara, I know of a guy in MN who had a severe case of anaplasmosis, who is now having trouble with Reynalds symptoms, the cold hands and feet. If you haven’t been tested for that TBD, it would be worth a shot.
It seems worthwhile to divide the non-responders into two sub groups. One who have few to no changes, and the other who have their symptoms worsen, which certainly can be a ‘response’. Within those who worsen there will be the challenge of learning who is facing a ‘normal’ progression of the disease due to failure of the treatment, and who is having a Herx reaction due to success of the treatment in killing some of the bacteria.
I had Lyme for 12 years before I was treated. When I was finally treated by a Lyme Literate Doctor, I was so sick that the treatment didn’t help much. Now 23 years later, I’m very ill and would be happy to be as sick as I was when I was first treated. I now have no tolerance for any antibiotics, am mostly bedridden, now live in FL where the doctors know almost nothing about Lyme disease. I am too immune compromised to fly up north to see a competent Lyme doctor. When I read literature by someone like Dr. Richard Horowitz or Dr. Joseph Burrascano I realize that the doctor I’m seeing, although he’s trying very hard, has good will and is very intelligent, just doesn’t have the experience of these doctors.
I get worse everyday. I try to keep my outlook positive. I have a wonderful husband and am grateful but I feel more and more isolated. I really don’t believe any meds really helped me and they sure don’t help me now. I really don’t know what to do.
Look into DESBIO…And check facebook for a support page. Iowa has a facebook page for lyme and my wife gets allot of support through this.
I live in an area that is not very up-to-date at all with Lyme disease and the treatment thereof so I would have to travel a great distance to get proper treatment. I was diagnosed With Lyme disease on April 7th 2014 I was on antibiotic treatment with an LLMD for the 1st year over an hour awa. Since then I am unable to afford a true Lyme doctor or the travel to get to onr. It s just getting worse just going to a rheumatologist, neurologist, cardiologist and so on and so forth what is a person to do without the funds to be able to go see a true LLMD and get the proper treatment that they need. I feel like I’m just a joke to them. I stay I’m my blacked out room most of the time because I just can’t stand the light or stress. I have a list a mile long of diagnosis, but no help. Any info would help 3 years and just getting worse by the day.
Tammy B.
Several people seem to be at a loss for treatment help. I recommend joining the Lyme forum on HealingWell.com. There is a commited block of people who have personal experiences to draw from, available to help with information from :what LLMDs are in your area, to what treatments have helped them, to whether a symptom seems likely to be Lyme or maybe co-infection related (or not). They are generally kind, sympathetic, and pretty frequently very well read on the subject of Lyme. There’s lots to learn by asking questions, and even more by searching the past threads. The moderators keep trolls out well too. Good luck to you all.
I think the treatment should be listed as well as the response. If they just had one med for acute lyme, that is one thing. If they are being treated for chronic lyme, the treatments vary so much that I think the statistics could be faulty. It is clear that it takes more meds that ever thought in the past to get chronic patients better. One is just not going to do it. Also, if co-infections are not treated, whether test proven or not, the results may not be as good as they could be.
This is not cookbook medicine!
I don’t know how long I had Lyme but it was a very long road. I was lucky I had a friend that watched me decline as a person physically and mentally. I was in a car accident on Christmas day and almost killed my daughter and myself. I was losing my sence of perception I thought I was driving fine but I was actually driving half in the oncoming traffic. I was so physically ill that I had to move to my daughters house so she could take care of me and my mentally challenged daughter. Just before I left my friend says please go and get tested for Lyme disease before you go. I didn’t want to go i didn’t want to get out of bed and have someone drive me but I had given my word and so I went. I proved positive for Lyme and was given the two weeks worth of antibiotics. I took the cure and made my move to my daughters. I was in bed with my daughter cooking and cleaning and driving me. Sometimes to the Er when I felt like I was dying. It is a year and a half and I am just finally feeling better. I still don’t do much but I can stay awake most of the day and am finally feeling like I am not going to die. It has been a harrowing. time but I have won the battle at least I have turned a corner for theory. It has been a year and a half in bed for complete rest.
I think it would be more helpful to know what treatment was provided for successful cases and whether or not the procedure was by IV infusion or oral tablets.