LYME SCI: Help! I’ve gotten a tick bite. Now what?

Tick season is in full-swing. How do I know that? I wake up practically every day to another text or email from a friend or relative telling me they had a tick bite.
Last week, I got a desperate call from a relative whose son had found a tick embedded in his skin after a camping trip. Both my cousin and her son are well aware of my daughter’s missed diagnosis and years’ long battle with Lyme and co-infections. Needless to say, they were in a panic. More about this later…
Of course the best thing is to prevent tick bites in the first place, but life happens and that’s probably why you’re reading this.
Here’s my advice if you have a tick bite:
Step 1 – Take a picture of the tick that bit you
Take a picture while the tick is still attached. This will show details of the tick that can help you identify it later. It will also show how deeply embedded the tick is, how engorged it is, and if a rash has already formed prior to you removing the tick and cleaning the area.
Step 2 – Remove the tick
- DO NOT squeeze, twist or squash the tick. Don’t burn it with a match or cover it with Vaseline or nail polish. Squeezing or agitating the tick may force it to expel more pathogens into your body.
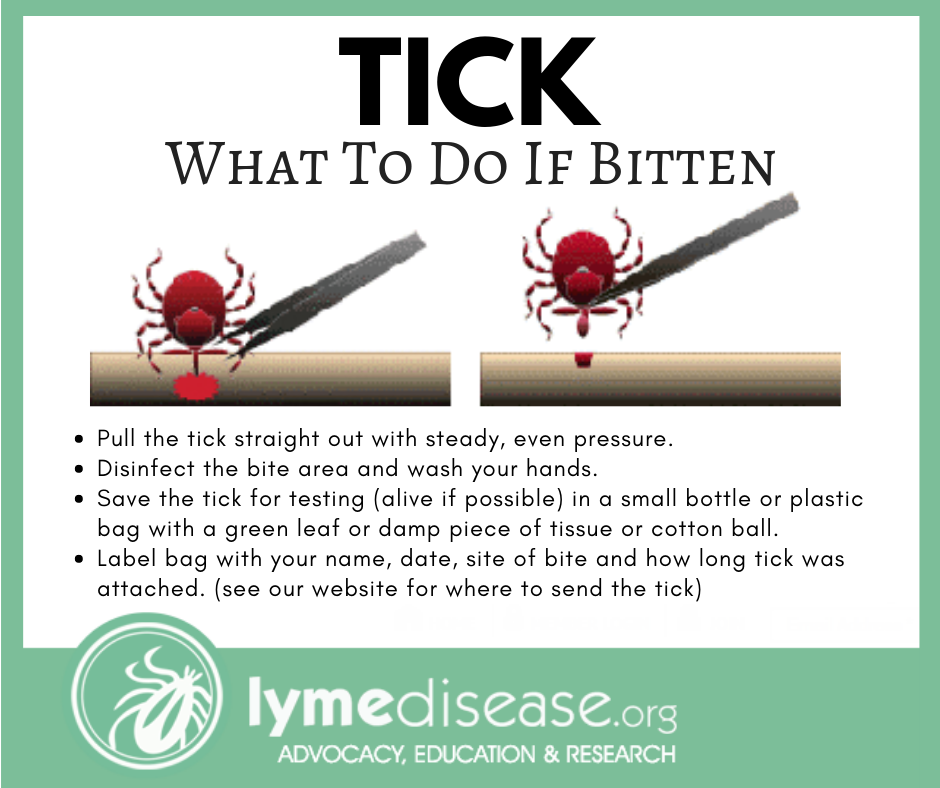
- Use fine-point tweezers or a special tick-removing tool. Grasp the ticks mouth parts or get as close to the skin as possible.
- DO NOT pull back sharply; this may tear the mouthparts from the body of the tick and leave them embedded in the skin.
- Pull the tick straight out with steady, slow, even pressure as pictured above. Be patient. The tick has long mouthparts. Pull steadily without twisting until you can ease the tick head straight out of the skin. It may take several seconds to a few minutes for the tick to unhook its mouth.
- Wash the bite area and your hands with soap and water. Disinfect the site with rubbing alcohol, then apply a triple antibiotic ointment or antiseptic.
Step 3 – Identify the tick you were bitten by
It’s important to identify the tick because different kinds of ticks can carry different bacteria, viruses, protozoa and parasites. (Lyme disease isn’t the only thing you need to worry about with ticks bites.)
There are two families of ticks found in the United States: Ixodidae (hard ticks) and Argasidae (soft ticks). Of the 700 species of hard ticks and 200 species of soft ticks found throughout the world, only a few are known to bite and transmit disease to humans. Knowing the type of tick will help you be aware of what possible symptoms to watch for.
Here’s how to identify a tick after a tick bite:
- After removing the tick, place it on a white piece of paper or clear tape, then take a picture of the front and back of the tick. DO NOT let it crawl away.
- Place the tick in a small plastic bag with a green leaf, damp cotton ball or moist piece of tissue. DO NOT place it in alcohol. Label the bag with your name, date, site of bite and how long the tick was attached.
- Use one of the following links to identify the tick. (If you can’t identify the tick, don’t worry, the testing lab will do it for you. Step 5 below)
- TickEncounter.org (you can submit a picture of the tick and they will identify for free)
- or you can download the TickTracker app on your smart phone.
[Optional: log your information in the app if you’d like advance knowledge of ticks in your area.]
Step 4 – See your primary care doctor
Before you get to the doctor, I highly recommend doing a little research about what tick-borne diseases are known to be in your area’s ticks.
There are a lot of misconceptions surrounding Lyme and tick-borne diseases. These are the main points I think you need to know before heading to the doctor:
The following are the most common misunderstood facts about tick bites:
- Ticks can transmit several pathogens (especially viruses) in as little as 15 minutes. While it is true that the longer a tick is attached, the more likely it is able to transfer Lyme, no one really knows how long a tick needs to be attached to transmit infection. A minimum attachment time has NEVER been established. It is dangerous to assume there is zero risk of contracting a disease if the tick has been attached less than 24 hours.
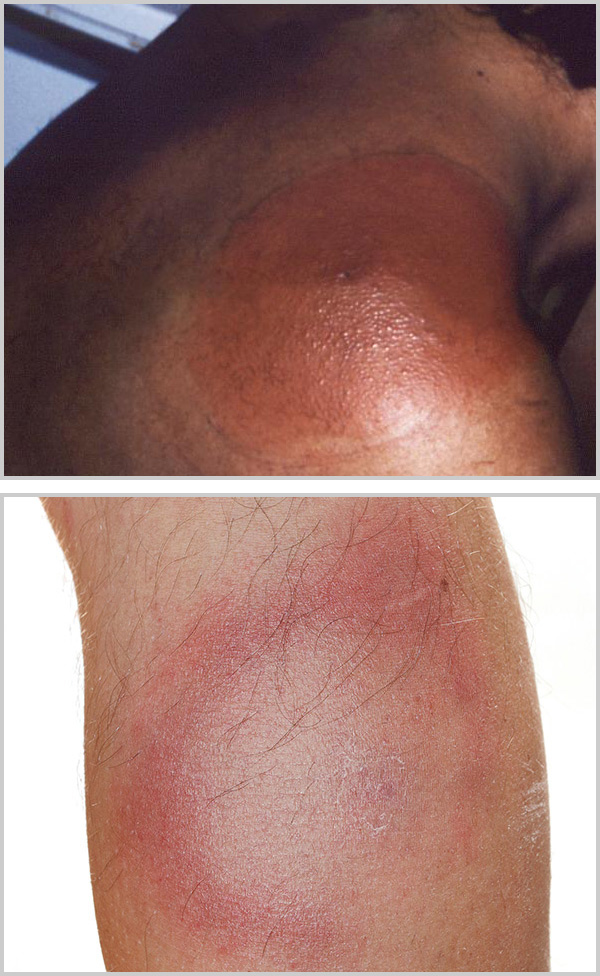
- Not everyone with Lyme gets a rash. Studies have shown that only 40-60% of Lyme patients will get an erythema migrans rash, and only 20-30% of those will present as the telltale bullseye rash. Several other tick-borne diseases may cause a rash. See here for Rocky Mountain spotted fever, and other common rickettsial rashes.
- A Single dose of Doxycycline is only effective at reducing the tick bite rash. It does not adequately treat any of the known pathogens. In fact, a single dose of doxy may only prevent the rash from surfacing, masking a crucial sign of illness. (Dr. Daniel Cameron does a great job of explaining the science here.)
- There is no point in testing for Lyme if you’ve just been bitten by a tick. First, Lyme disease is a clinical diagnosis based on signs and symptoms and history of possible exposure to infected blacklegged ticks. Second, the test for Lyme is prone to false-negatives, especially in the first 4-6 weeks, before the body has had a chance to produce the antibodies that are detected by the standard test. Each tick-borne disease requires a different test, and some of them are more accurate than others. Testing the tick can help you know what you’ve been exposed to. More about Lyme disease testing here:
Step 5 – Start Tick Bite Treatment
Rather than give medical advice about recommended treatment, I’m going to quote the International Lyme and Associated Diseases Society (ILADS – how to handle a tick bite):
“ILADS recommends that prophylaxis (preventive treatment) be discussed with all who have had a blacklegged tick bite. An appropriate course of antibiotics has been shown to prevent the onset of infection.
When the decision is made to use antibiotic prophylaxis, ILADS recommends 20 days of doxycycline (provided there are no contraindications). The decision to treat a blacklegged tick bite with antibiotics often depends on where in the country the bite occurred, whether there was evidence that the tick had begun feeding, and the age of the person who was bitten. Based on the available evidence, and provided that it is safe to do so, ILADS recommends a 20-day course of doxycycline.
Patients should also know that although doxycycline can prevent cases of Lyme disease, ticks in some areas carry multiple pathogens, some of which, including Babesia, Powassan virus, and Bartonella, are not responsive to doxycycline. This means a person could contract a tick-borne illness despite receiving antibiotic prophylaxis for their known bite.
ILADS recommends against single-dose doxycycline. Some doctors prescribe a single 200 mg dose of doxycycline for a known bite. However, as discussed in detail in the guidelines, this practice is based on a flawed study that has never been replicated.
Read more in the ILADS treatment guidelines.
Step 6 – Mail The Tick For Testing
Knowing what diseases the tick is carrying (if anything) will either give you peace of mind or provide valuable clues as to what symptoms to watch for and which disease(s) to treat. One thing we know for sure, early treatment for any tick-borne disease is the key to full recovery. Delaying treatment by as little as 3-4 weeks can increase your odds of having long-term damage.
Many states offer free tick testing, although they may only test for one or two pathogens. You can call your local public health department and see what they offer.
I recommend sending the tick in for testing to determine if the tick is carrying any pathogens that can lead to tick-borne illness. If you can not find free testing, I recommend one of following laboratories:
- IGeneX (tests individually for up to 8 pathogens, $75 each)
- Tick Report (test for up to 23 pathogens, $50 – $200)
- Ticknology (test for up to 11 pathogens, $25 – $45)
Step 7 – Start Tracking Symptoms From Your Tick Bite
Immediately start tracking any symptoms that are out of the ordinary. On a calendar or diary, write down any flu-like symptoms, headache, fever, ringing in the ears, weird numbness or tingling, facial palsy, nausea, migrating pain, joint swelling, night sweats. Seriously, write down anything that is not normal for you. Symptoms of tick-borne diseases can begin anywhere from 1-3 days to 4-6 weeks after the bite. (More about tick bite symptoms to watch for)
Observe the bite site over the next three weeks for any signs of a rash. Take pictures of any visible changes anywhere on your body (not just the bite site). Place a quarter or tape measure next to any rash for size reference.
Let your doctor know immediately of any signs of illness. (Check your symptoms for Lyme.)
Step 8 – Await The Results Of Your Tick Test
Most of these results are coming back within a week. During that time, monitor your symptoms and notify your doctor if anything gets worse. If you are on doxycycline, you may actually avoid getting sick.
Once the results come back you will need to discuss what to do. If the tick is positive, you will want to stay on treatment. Many ILADS practitioners will prescribe 4-6 weeks for early Lyme. Other pathogens, like Anaplasma or Ehrlichia, will be treated for a different duration. Babesia is treated with an entirely different medication.
If the tick test is negative, that doesn’t mean you are out of danger. It depends on your exposure and your symptoms. One thing to consider is how long you were exposed to the ticks and whether there could have been another bite that you did not see. Even though one tick is negative, another tick could have been positive. This is something you will really need to discuss with your medical provider.
What happened to my relative when they got a tick bite?
To finish the story about my cousin’s son. I basically told them everything I have spelled out above. Just as I predicted, when they got to the doctor, he said, “If the tick hasn’t been attached for over 24 hours you’ve got nothing to worry about.” STRIKE ONE
They showed him the photograph of the embedded tick and the red circular rash that had started to form. The doctor said, “Well, because you’ve got a rash, I’m going to give you a single dose of doxycycline and that should cover it.” STRIKE TWO
They explained what they had learned and the doctor was actually very interested. They established a rapport. In the end, they left with a 20-day supply of doxycycline and their doctor wanting them to come back with the full tick report and any information they had to share. He was interested in learning more. A HOME RUN!
- Tick Removal | Ticks | CDC https://www.cdc.gov/ticks/removing_a_tick.html
- Barker S., & Murrell, A. (2004). Systematics and evolution of ticks with a list of valid genus and species names. Parasitology, 129(S1), S15-S36. https://doi.org/10.1017/S0031182004005207
- Vayssier-Taussat M, et al (2016). Co-infection of Ticks: The Rule Rather Than the Exception. PLO Neglected Tropical Disease. https://doi.org/10.1371/journal.pntd.0004539
- Transmission | Powassan | CDC https://www.cdc.gov/powassan/transmission.html
- Cameron D, Johnson L, Maloney E. (2014) Evidence assessments and guideline recommendations in Lyme disease: the clinical management of known tick bites, erythema migrans rashes and persistent disease, Expert Review of Anti-infective Therapy, 12:9, 1103-1135, https://doi.org/10.1586/14787210.2014.940900
LymeSci is written by Lonnie Marcum, a Licensed Physical Therapist and mother of a daughter with Lyme. Follow her on Twitter: @LonnieRhea Email her at: lmarcum@lymedisease.org .




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page