W hen I learned that I had Lyme disease way back in 1987, no one knew that babesiosis, ehrlichiosis, or other tick-borne infections could co-infect people and potentially exacerbate one’s illness. Simply put, they weren’t on anyone’s radar. But it makes sense that Ixodes ticks, the primary vectors of these diseases worldwide that feed on several hundred different species of lizards, birds, and mammals, could acquire many blood-borne organisms from their hosts. In fact, a 2014 Chinese study found that locally collected ticks transmitted 237 different bacteria to lab-raised rats. The authors concluded there is “unambiguous evidence that there are as-yet unidentified pathogens associated with ticks, [which] increases the risk of multiple infections in humans, [leading] to more severe clinical manifestations.”
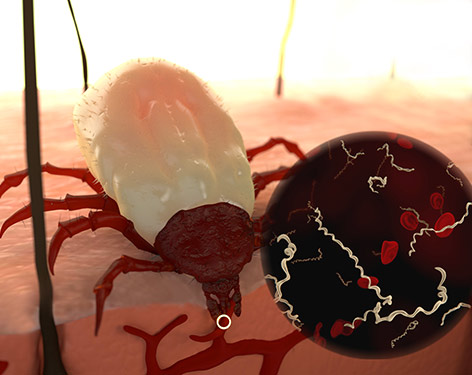
The pathogens ticks ingest during their blood meal from wildlife—Lyme disease spirochetes, Powassan virus, Bartonella, Ehrlichia, and others—develop strain- and species-specific variations as they co-evolve with their primary vertebrate hosts or tick carriers in a given geographic region. Taxonomic studies demonstrate complex interrelationships among strains and species of such pathogens around the world—not surprisingly, as many are carried by birds as well as mammals. And scientists are discovering new microbes all the time. The field of vector-borne disease is exploding. A cursory search of “tick-borne diseases” on PubMed reveals more than 700 published articles from Korea, Turkey, Uruguay, the Congo, and other countries published in the past year alone.
“There are hundreds of possible combinations just from the pathogens we already know about, to say nothing of those that await discovery.”
The fact that the picture remains incomplete has serious implications for patient care. In the best of times, it takes months or years for scientific research to trickle down to the trenches. For example, few physicians know that because of its great diversity of climate and vertebrate hosts, my home state—California—hosts 48 of the 86 species of ticks found in the United States. My state is also home to more species of Lyme disease and relapsing fever-group Borrelia than any other. Nevertheless, at the Integrated Pest Management meeting I attended in Washington, D.C., In 2016, I took the microphone to complain that several of the researchers had shown only the eastern half of the country on their maps. (They promised to do better next time.) My point is, if doctors aren’t informed where these diseases occur, they can’t diagnose them.
If you are one of the unlucky patients having one or more co-infections, please know that there are hundreds of possible combinations just from the pathogens we already know about, to say nothing of those that await discovery. But patients often cannot obtain treatment without a positive test result and there are no commercially available tests for detecting most of these bugs! There are other obstacles.
For instance the Centers for Disease Control and Prevention (CDC) does not encourage the belief that Bartonellosis can be transmitted to humans by ticks. Bartonella species have been found in patients with other tick-borne diseases, but so far no one has been able to meet the official definition of “transmission” required by evidence-based scientific standards. Hence, it is likely that millions of people afflicted by tick-borne illnesses are not being treated properly because doctors have not been able to diagnose them.
This issue of The Lyme Times provides an overview of some of the recent discoveries, and takes a closer look at some of the more common human co-infections. We will be adding to this issue as new information becomes available. The important point to emphasize is that our knowledge of tick-borne infections is still in its infancy. We urgently need more sensitive tests and more effective treatments. LymeDisease.org is committed to pushing for more research, and to giving patients a voice in these vital issues that affect their lives.



















